The abuse of science: the anti-science movement using cherry-picking to pretend SARS-CoV-2 has similar effects to HIV
How the "World Health Network" and all associated have lost even the last bit of credibility
Indeed, any scientist with a basic understanding of immunology or virology would likely have fallen off their chair reading this, wondering if the American Journal of Preventive Medicine had lost all sense of rigor.
Are there meaningful commonalities between SARS-CoV-2 and HIV? Superficially, yes: both are viruses, both can cause disease and death, and both have triggered global pandemics and health scares. But the similarities end there. COVID-19 and AIDS are fundamentally different diseases. The viruses belong to entirely different families, exhibit distinct biological behaviors, infect different host cells, and are transmitted via different routes. Importantly, SARS-CoV-2 is vaccine-preventable, whereas HIV still is not.
Some people from fields like sociology, chemistry, nuclear medicine, or physics suddenly act as if they have deep insights into immunology and virology. Do they even understand the fundamental differences between HIV and SARS-CoV-2, particularly in the context of mammalian biology?
Of course, if you cherry-pick poorly designed papers, ignore proper context, omit or misuse controls, and misinterpret results, you can construct almost any narrative and call it “science.” But it isn’t science—it’s attention-seeking activism and anti-science posturing.
Let’s highlight the main points. One political statement may be correct—but the rest? Unsubstantiated claims that largely contradict established scientific knowledge and data.
Of course, we can go through each argument and each reference…. with 200 references from low impact journals, predatory journals, general webpages, press releases, etc, it is a big job.
Introduction: Why compare HIV and SARS-CoV-2?
Why indeed. The comparison largely makes no scientific sense. Yes, both are viruses—though from entirely different families: HIV belongs to the Retroviridae family and the genus Lentivirus, while SARS-CoV-2 is a coronavirus. Both were novel to humans, caused significant health scares, and influenced public health policies. And that should be where the comparison ends.
Unfortunately, the authors—Spela Salamon, Arneaux Kruger, Deborah Lupton, Etheresia Pretorius, Andrew G. Ewing, and Yaneer Bar-Yam—went much further, and far beyond what is scientifically justified.
For example, they claim:
“HIV-1 and SARS-CoV-2 infections typically present with ‘cold-like’ symptoms days after infection.”
This is a very broad and misleading statement. These symptoms are not caused directly by the pathogens themselves, as the authors imply, but by the host immune response. In fact, almost all pathogens activate the immune system, often producing similar cold- or flu-like symptoms, regardless of the virus. Suggesting otherwise risks confusing the reader and overstating the uniqueness of SARS-CoV-2 or HIV.
The authors also state:
“Notably, similarities in the surface glycoproteins of both viruses have led to a higher occurrence of HIV false-positive results in individuals with antibodies against SARS-CoV-2 Spike protein (7).”
The referenced paper fails to provide any mechanistic link, which should be supplied here. The WHN collective claims shared epitopes between HIV and SARS-CoV-2 but does not identify which epitopes. What the study actually found: in a small cohort, the false-positive rate in the general population was 1.3% (expected: 0.4%), and in SARS-CoV-2-infected samples, it was 1.4%. That is it—no further evidence, no support for the sweeping claims made by the WHN authors.
Similarly, they claim:
“Especially since the emergence of Omicron sublineages, reinfections are likely to occur at least yearly if not several times per year without protective measures (10, 11).”
Again, the cited references are not linked properly in their paper. Examining the studies:
Reference (10) analyses waning neutralising antibodies after vaccination during 2020–2021; it does not support claims of yearly reinfections, nor does it compare to HIV.
Reference (11) examines infection effectiveness from July 2020 to November 2022, again focusing on antibody waning during the pandemic, but provides no evidence for annual reinfection rates.
Once more, the WHN collective overstates the findings and draws connections to HIV that are entirely unjustified.
The authors further claim:
“Especially in older individuals, previous Omicron infection can increase the risk of reinfection with the newer variants (12).”
This study is limited to elderly individuals in care homes, where confounders are numerous. Its findings cannot be extrapolated to the general population, who develop immune memory from infection. This principle is well-established for all pathogens, not just SARS-CoV-2. Therefore, the statement is false and contradicted by substantial evidence.
They continue:
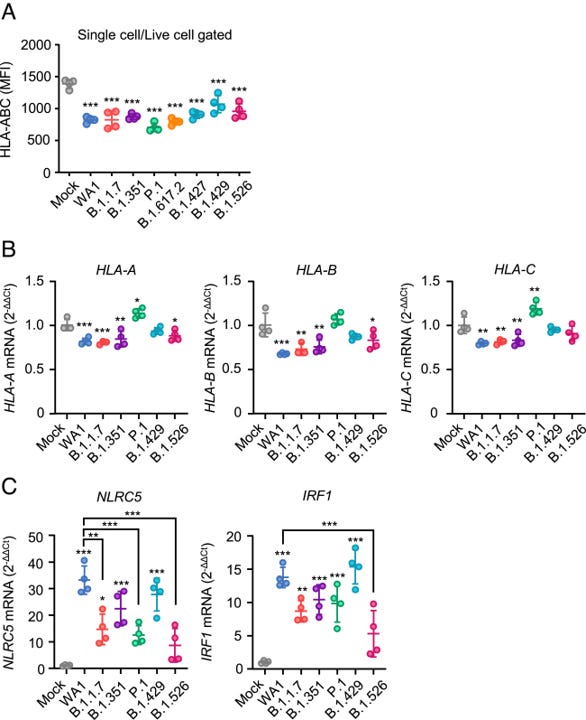
“Omicron subvariants exhibit enhanced evasion from T cell recognition (13)(14).”
This claim is unsupported by the cited references:
Reference (13) is an MDPI journal paper that does not measure T cell responses at all.
Reference (14), a PNAS study, examines MHC I downregulation, a phenomenon common to many viruses. While pathogens may reduce MHC expression to evade detection, NK cells counteract this, preventing effective immune evasion. SARS-CoV-2 does not meaningfully bypass T cell surveillance in this manner.
In short, the WHN collective misinterprets or overstates the findings, presenting them as unique to SARS-CoV-2 when they are neither novel nor generalizable.
The claims escalate further:
“In addition, BA.4 and BA.5 subvariants and their descendants have evolved improved suppression of innate immunity compared with earlier subvariants BA.1 and BA.2. Even more recent subvariants BA.2.75 and XBB lineages also exhibit enhanced suppression of innate immune activation (15).”
This is a clear overinterpretation of viral evolution, which naturally adapts to its host. The cited paper (15) actually states:
“Our data suggest that convergent evolution of enhanced innate immune antagonist expression is a common pathway of human adaptation and link Omicron subvariant dominance to improved innate immune evasion.”
In other words, these changes are expected adaptations, not evidence that SARS-CoV-2 is evading the immune system in any unprecedented or alarming way. Regardless of the variant, our immune system effectively controls the virus, which explains why severe disease, hospitalizations, deaths, and secondary complications have markedly decreased, and why additional widespread interventions are no longer required.
Once again, the WHN collective demonstrates a lack of understanding of immunology and virology, presenting normal viral evolution as if it were uniquely dangerous.
“Both infections can cause chronic, multisystemic conditions characterized by immune dysfunction. HIV/AIDS typically leads to permanent, life-threatening immune system damage that develops after several years (5). SARS-CoV-2, by contrast, exhibits a wide range of effects which develop in weeks to months, and sometimes persist (16–21).”
Yes, many outcomes are theoretically possible, but most do not occur, or carry very low risk. The WHN collective emphasizes these possibilities to create the impression that severe outcomes are common, which is misleading.
They escalate this further:
“with reinfections compounding organ damage and functional decline (22–24).”
This reflects a recurring WHN tactic; suggesting that SARS-CoV-2 infection and COVID-19 vaccines are ineffective or harmful, mirroring the arguments often made by anti-vaccination groups. If taken literally, this claim would imply SARS-CoV-2 is the first pathogen in history that not only fails to induce immune memory (which is demonstrably false, as antibodies and T cells are measurable after infection and vaccination), but also worsens outcomes with each reinfection, a biologically unsupported scenario.
Examining the references:
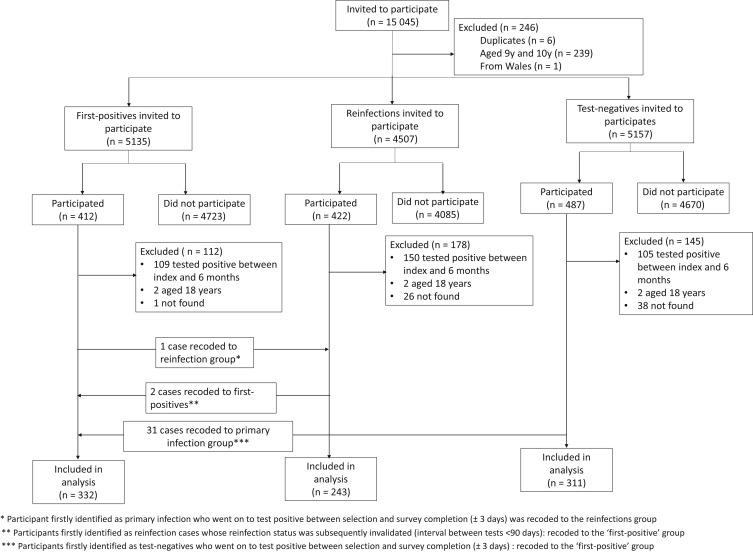
(22) compares children with 0, 1, or 2 SARS-CoV-2 infections. No significant differences were observed between those infected once versus twice. Moreover, the study relied on an online questionnaire with only a 10% response rate, introducing severe bias and making it unsuitable to substantiate claims of compounding organ damage.
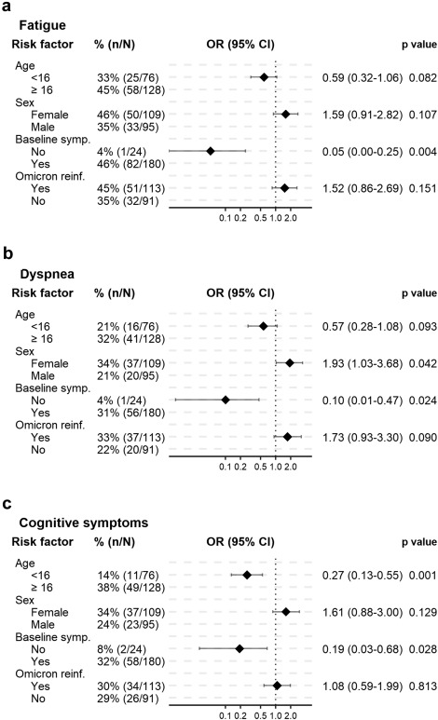
(23) This study compares children and adolescents infected during the Delta and Omicron waves, using an online questionnaire with only a moderate response rate. The findings suggest that adolescents were more likely to report symptoms and that higher antibody levels correlated with Long COVID–associated symptoms. However, nowhere does this demonstrate that reinfections cause worse outcomes. The WHN collective misrepresents these findings to support their narrative of cumulative organ damage.
(24) reports on only 33 subjects with recurrent, symptomatic infections; a highly selective cohort including only those reinfected and symptomatic. This group is not representative of the general population, and the study does not provide evidence that reinfections worsen outcomes.
In short, across references (22–24), the WHN collective fails to substantiate their claims that reinfections compound organ damage or functional decline. Their interpretation overstates the data and misleads readers, using small or biased cohorts to support a narrative that is not supported by the evidence.
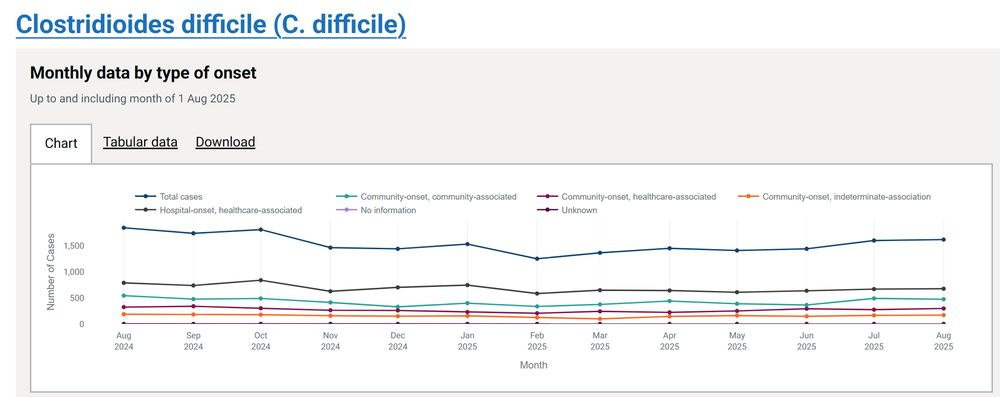
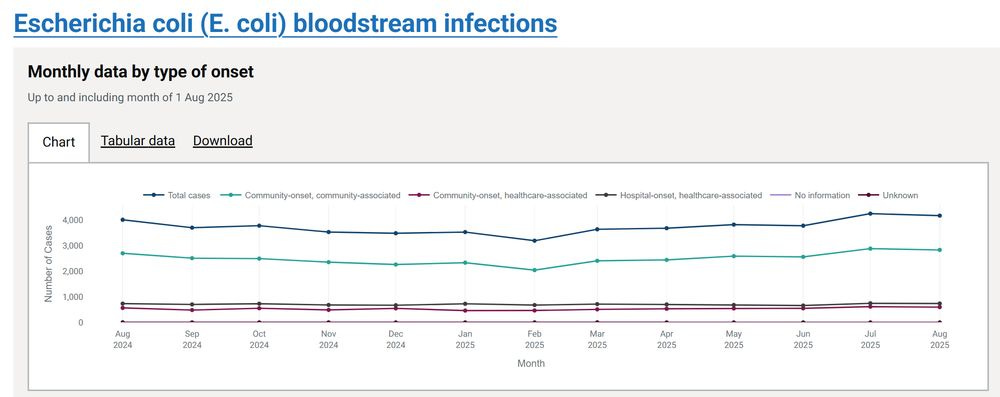
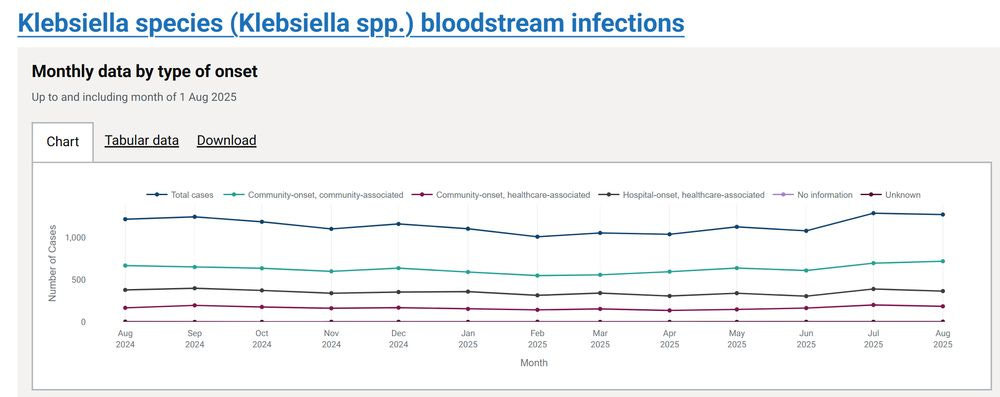
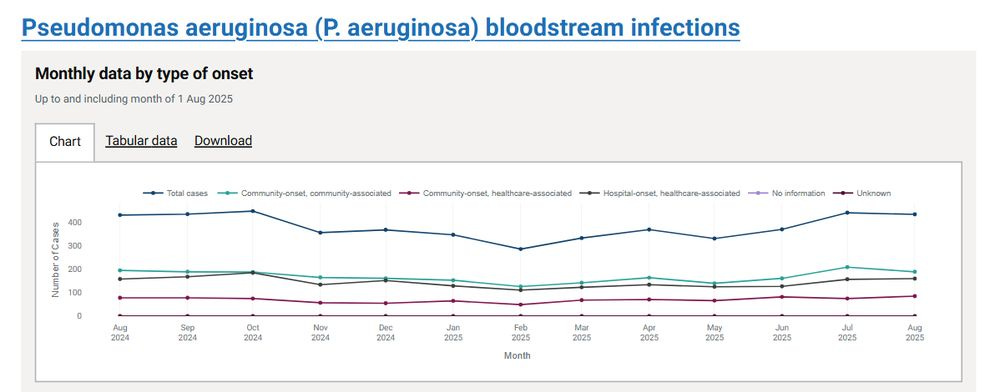
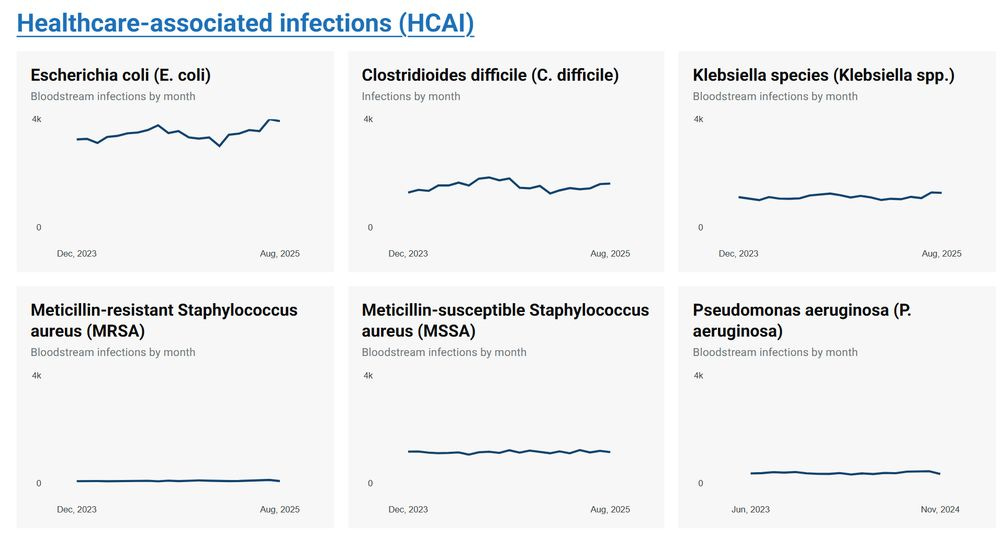
The WHN collective claims: “We are witnessing population-wide increases in many infections, including typical opportunistic infections (25), after widespread infections by SARS-CoV-2—consistent with what would be expected from long-term or cumulative immunodeficiency after COVID-19 infections (26, 27).”
The data? Again, no substantiation of the WHN claims.
(25) Cherry-picks a single pathogen. True immunodeficiency would manifest across a broad range of opportunistic infections, which is not observed.
(26) A report from a company selling air purifiers mentions some diseases (dengue, etc.) increasing due to climate change—not SARS-CoV-2-induced immunodeficiency.
(27) UKHSA Notifications of Infectious Diseases show no unusual surges in infections post-COVID.
Nevertheless, the WHN authors continue:
“At the population level, these increases in infections are driven by both reductions in individual immune system competence and the compounding effect of greater exposure to circulating pathogens, linked to weakened immune function. The evidence that this may largely be due to the immunological effects of COVID-19 infections is accumulating (28–32).”
A closer look at these references shows no substantiation:
(28) A commentary on immune imprinting; theoretical and often misunderstood, not evidence of immunodeficiency. It is not original antigenic sin, a theoretical frame work, shown to not hold for SARS-CoV-2.
(29) A study on oral microbiota dysbiosis, reflecting normal inflammatory responses, not chronic immune damage.
(30) A review; it does not show weakened immunity.
(31) An MDPI paper reporting T and B cell activation and subsequent memory formation; all physiological, healthy immune responses, not impairment.
(32) Commentary on “immune debt,” describing temporal surges after reduced exposure due to public health measures, not COVID-induced immunodeficiency.
The WHN collective repeatedly misinterprets and misuses the literature. Their claims of post-COVID immunodeficiency at a population level are unsupported, misleading, and demonstrate a profound misunderstanding of immunology.
The WHN collective claims:
“No comparable treatment exists for Long COVID or persistent SARS-CoV-2 infection, and curative, reservoir-clearing antiviral therapies or sterilizing vaccines remain unavailable for either disease.”
This is an unfounded assumption. There is no evidence that Long COVID is caused by viral persistence or reactivation. Key points:
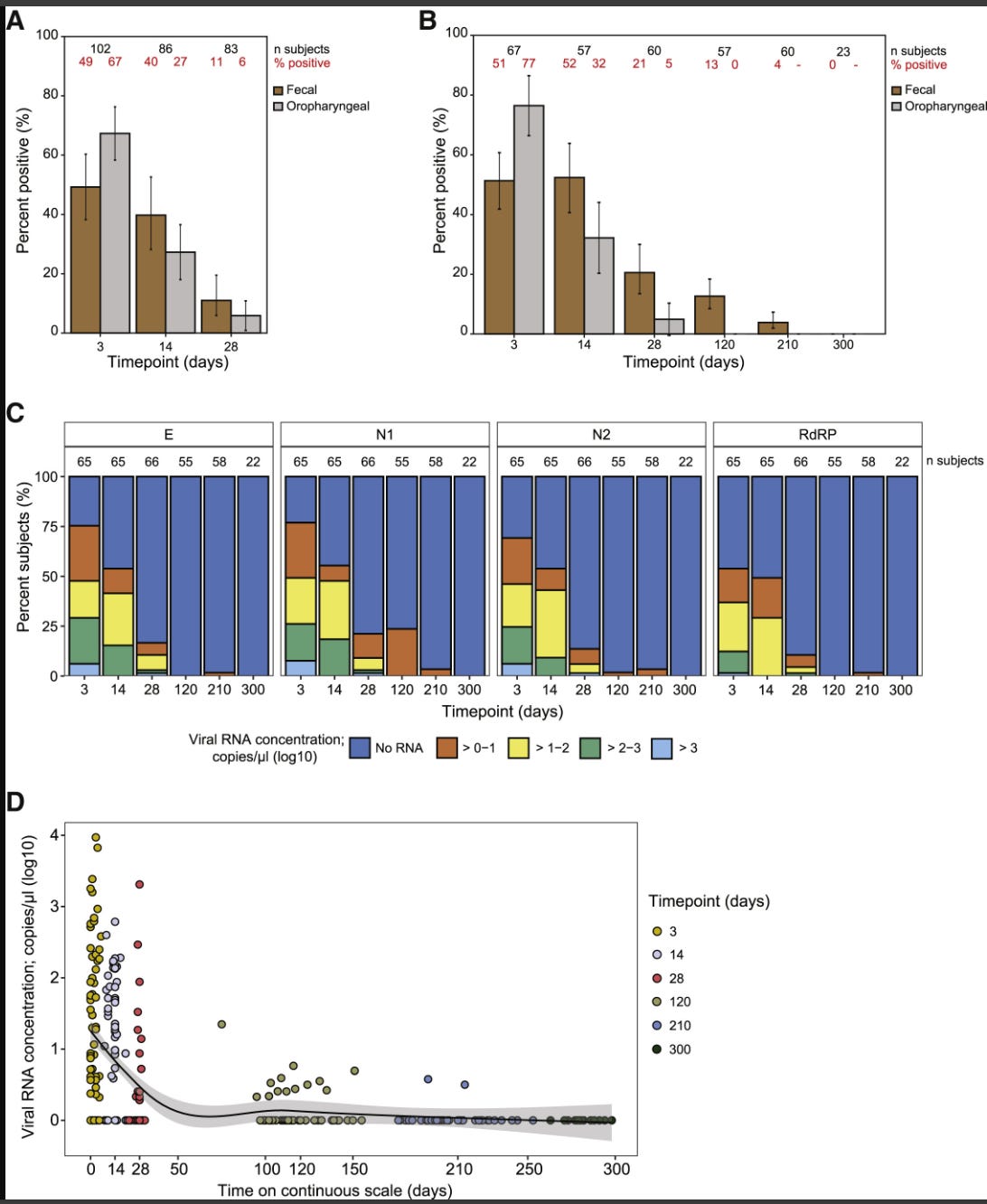
No persistent virus has been detected in typical Long COVID patients, only viral debris, such as RNA or protein fragments.
Antiviral or antibody therapies have not shown clinical benefit for Long COVID.
Viral debris is also found in individuals without Long COVID symptoms, indicating its presence is not causal.
Individuals with prolonged infection due to genetic or acquired immunodeficiency may harbour virus for longer, yet do not develop Long COVID, further undermining the claim.
Thus, the statement about the lack of “curative therapies” presumes a mechanism, persistent virus, that has not been substantiated by evidence.
Methods
The WHN collective describes their work as a “narrative review.” In reality, it is far from a proper scientific review. It reads more like a one-sided fantasy story, lacking evidence and rigorous methodology.
Their claim of having conducted “a comprehensive literature search” is misleading. In practice, this appears to mean: Google for papers that support preconceptions, cherry-pick results, and twist, misinterpret, or overinterpret them while ignoring the rest of the evidence. The authors openly acknowledge their bias when they state: “Given emerging evidence that SARS-CoV-2 may induce chronic immune dysfunction…”
Yet, there is no evidence for such chronic immune dysfunction in the general population post-infection. The attempt to compare SARS-CoV-2 to HIV and AIDS is not only scientifically unfounded but also harmful, as it:
Spreads unnecessary anxiety among readers.
Undermines trust in science.
Misrepresents both diseases in ways that are potentially dangerous.
In short, this is an anti-science narrative masquerading as a review and should never have been published.
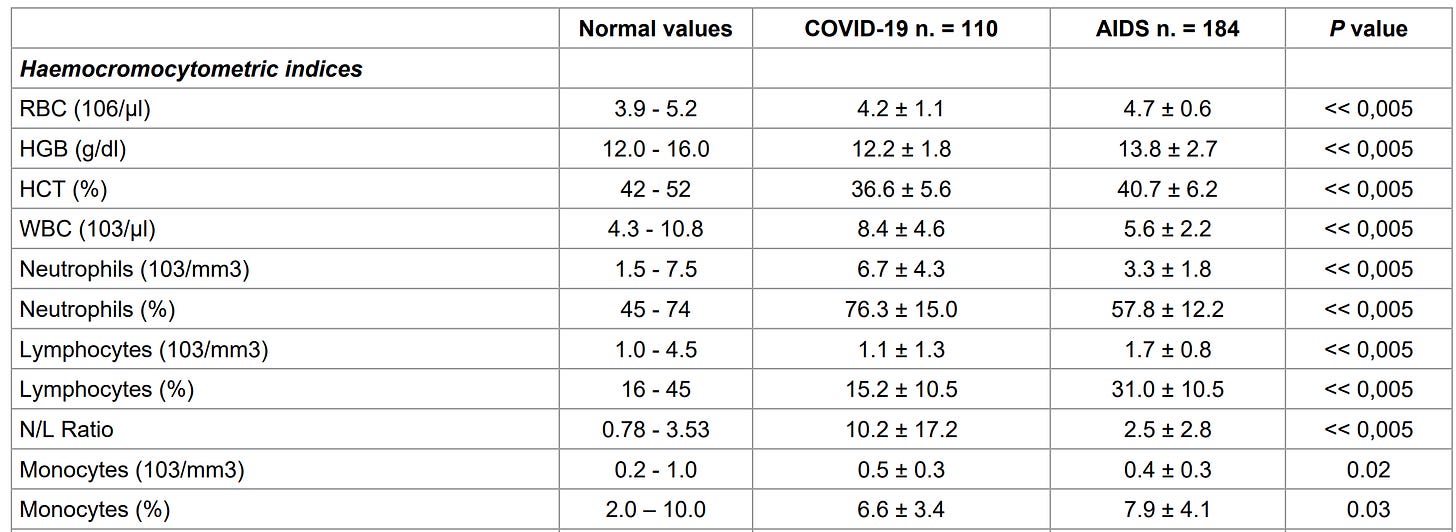
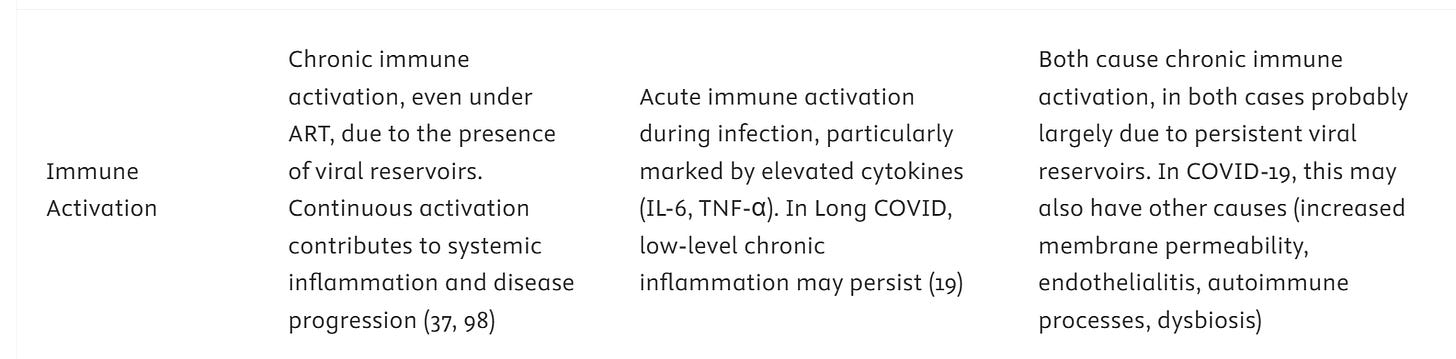
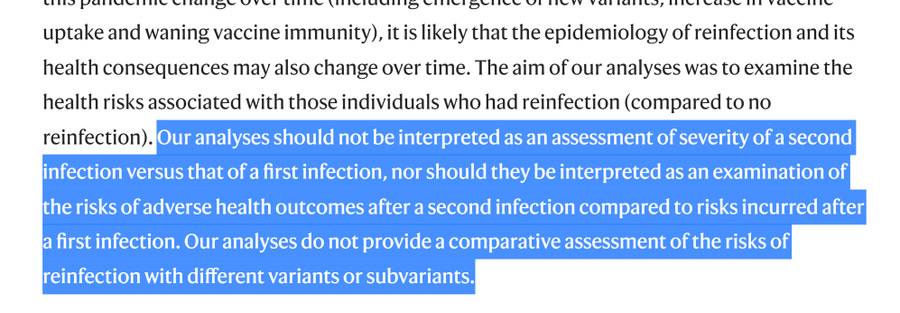
Immune System Dysfunction in HIV and SARS-CoV-2: Parallels and Divergences
This section begins with well-established facts: HIV infects immune cells, primarily CD4 T cells, although not exclusively, as macrophages also serve as a viral reservoir (a helpful plain language guide here). For clarity, there are actually two HIV viruses: HIV-1, the most prevalent and widely studied, and HIV-2, which appears to be gradually disappearing.
The WHN collective then engages in an abuse of scientific uncertainty by stating:
“the long-term impact of SARS-CoV-2 infections on immune function remains uncertain.”
This phrasing exploits the inherent scientific openness, where we acknowledge that new methods and data may refine our understanding. However, uncertainty does not imply ignorance or justify alarmist claims. SARS-CoV-2 was sequenced in early 2020, is a coronavirus, and contains no unknown genes or functions that would fundamentally alter its behaviour compared with other coronaviruses that regularly infect humans. The WHN collective fails to substantiate this broad and worrying implication, and their framing is misleading rather than informative.
The WHN paper claims:
“A single SARS-CoV-2 infection can induce a broader spectrum of immune system dysregulation in days to weeks (Figure 2), including but not limited to T cell depletion and functional exhaustion of T cells – see Table 1 for more details (16).”
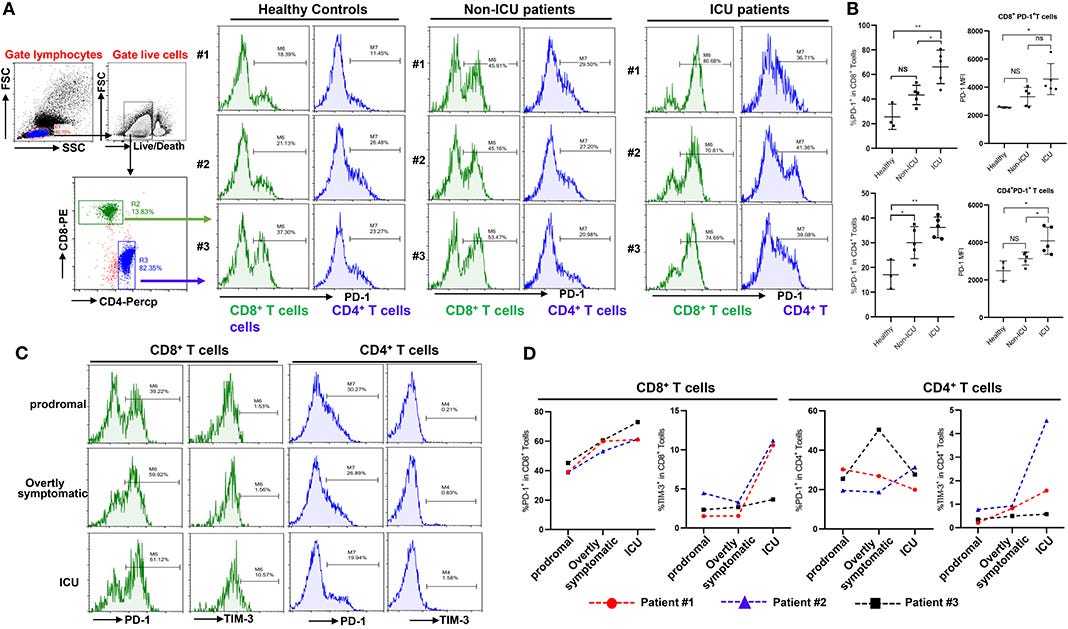
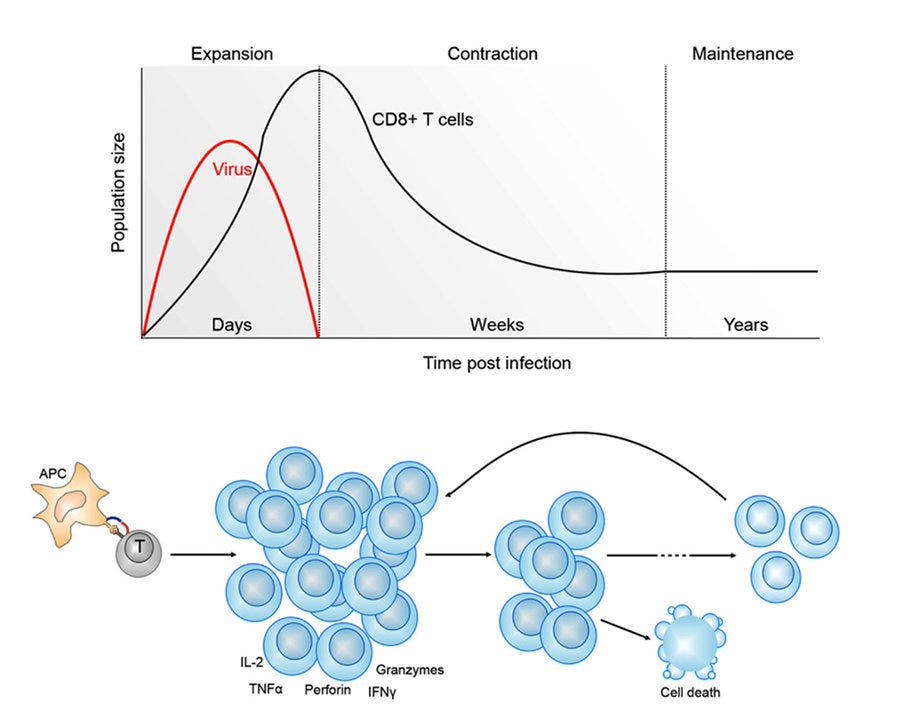
Reference (16) is a Frontiers paper whose title mentions “functional exhaustion.” But what does exhaustion actually mean? It is not fatigue or extreme tiredness. Instead, it refers to the upregulation of immune checkpoint molecules such as LAG3, TIM3, PD-1, TIGIT, and CTLA-4. This is a normal regulatory mechanism: if an immune response becomes overly aggressive, these molecules tone it down to prevent collateral tissue damage.
Exhausted T cells are common in chronic conditions such as cancer, and can be reactivated experimentally by blocking interactions between these markers and their ligands—a Nobel-prize-winning discovery in 2018. Even in acute immune responses, precursor exhausted T cells appear as part of physiological regulation (ref and ref). Many memory T cells, especially tissue-resident T cells, naturally express these markers (nicely shown in this preprint), which is also the reason for some side effects observed with immune checkpoint inhibitor therapies. In short, the presence of exhausted T cells is physiological and does not indicate dysfunction.
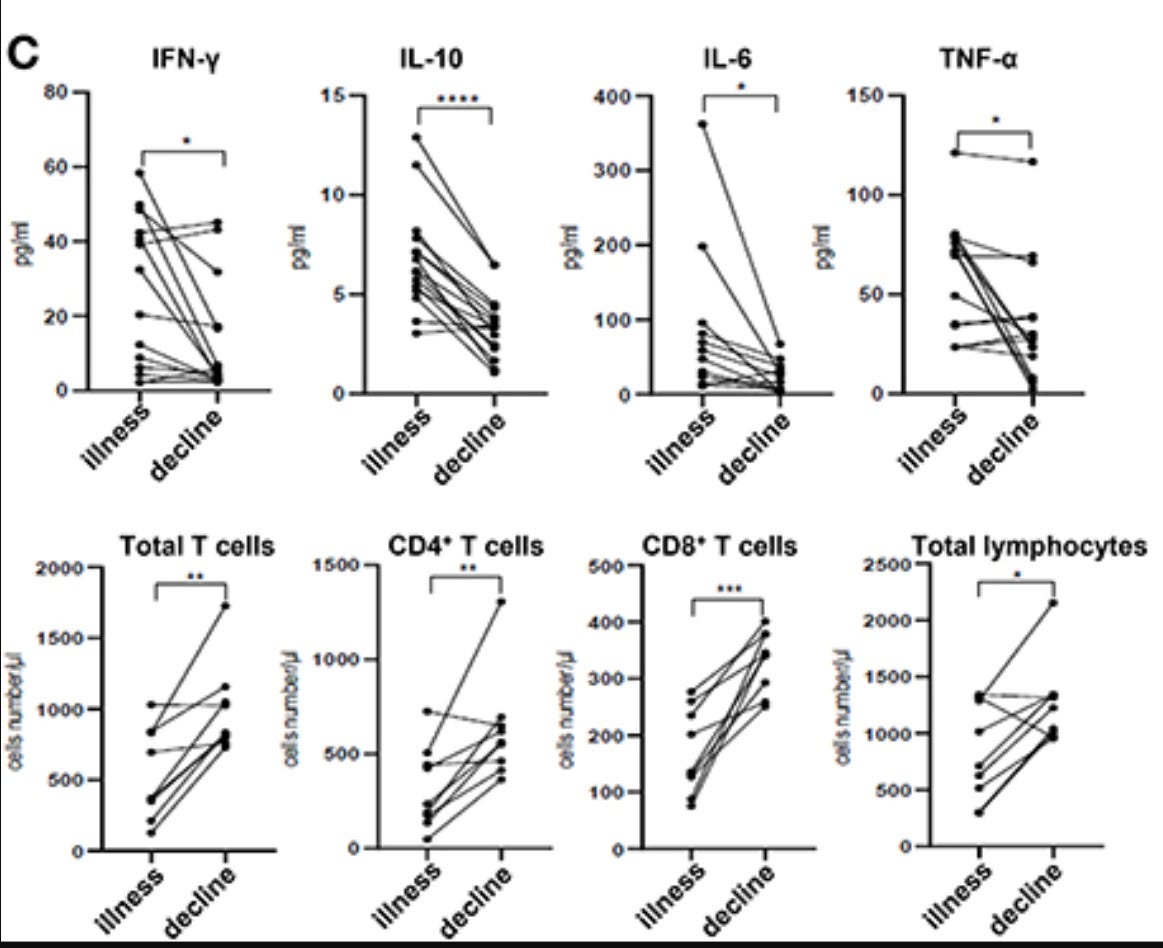
What did the study actually show? The cohort included subjects from December 2019 to January 2020, the first pandemic wave, without vaccines or prior immune memory. Participants ranged from 5 days to 97 years, and the study focused on acute infection. In elderly patients, more severe inflammation correlated with reduced blood T cell numbers and higher cytokine levels. As patients recovered, cytokines decreased and T cell numbers rebounded.
Regarding “exhaustion”: these cells were temporarily more abundant during inflammation, acting to protect the host from immune-mediated damage. They are fully functional and disappear once the inflammatory response resolves. Importantly, these T and B cells are SARS-CoV-2-specific, expanded massively from a tiny precursor population. They do not represent the entirety of your immune system or other pathogen-specific T and B cells. The WHN collective misinterprets this, implying that all immune cells are affected, which is incorrect.
This is a perfect illustration of Brandolini’s law: it is easy to make sensational claims, but explaining context, mechanism, and actual data requires much more nuance. The table provided in the WHN paper fails to capture this complexity.
The table:
HIV versus SARS-CoV-2: T cell depletion
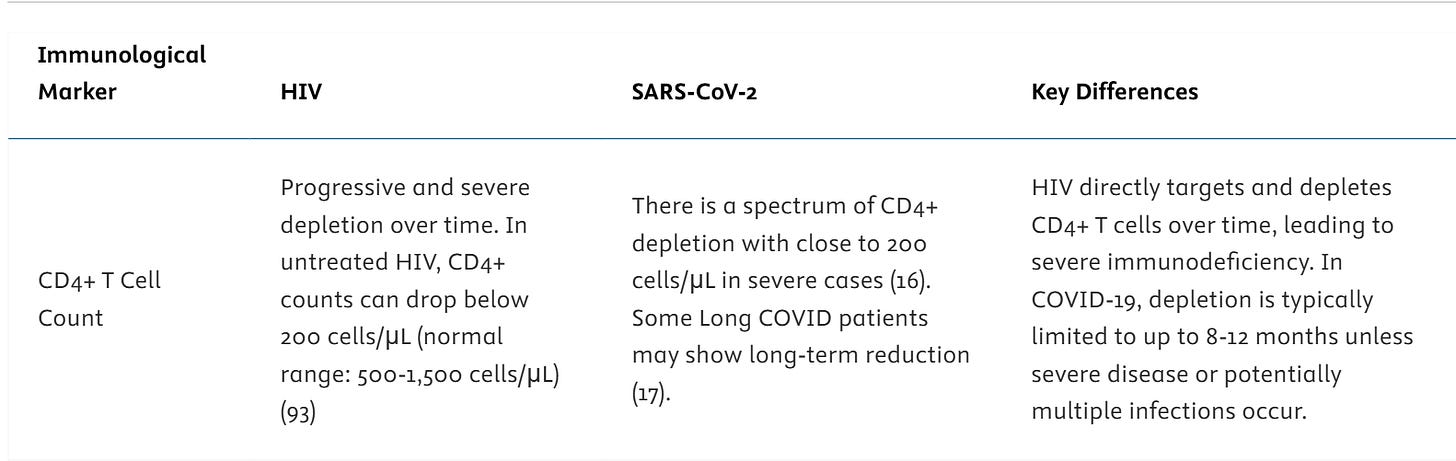
For HIV, the science is clear: CD4 T cells are directly infected and destroyed by the virus, leading to the progressive immunodeficiency that defines AIDS. This is well-documented and the numbers of CD4 T cells drop continuously over time.
For SARS-CoV-2, the situation is entirely different. Like any acute inflammatory event, whether caused by infection, trauma, or ICU-level illness, T cell numbers can transiently decrease. This reduction is a well-known prognostic marker in acute inflammation and is not specific to SARS-CoV-2. Importantly, SARS-CoV-2 does not infect T cells directly, nor does it cause long-term depletion.
Reference (16), as discussed above, does not provide evidence of SARS-CoV-2-specific T cell depletion. Reference (17) is even weaker: published in a very low-impact journal (IF 0.237) with predatory characteristics, not indexed in PubMed. The paper shows no abnormal values and contributes nothing to substantiate claims of virus-specific T cell loss.
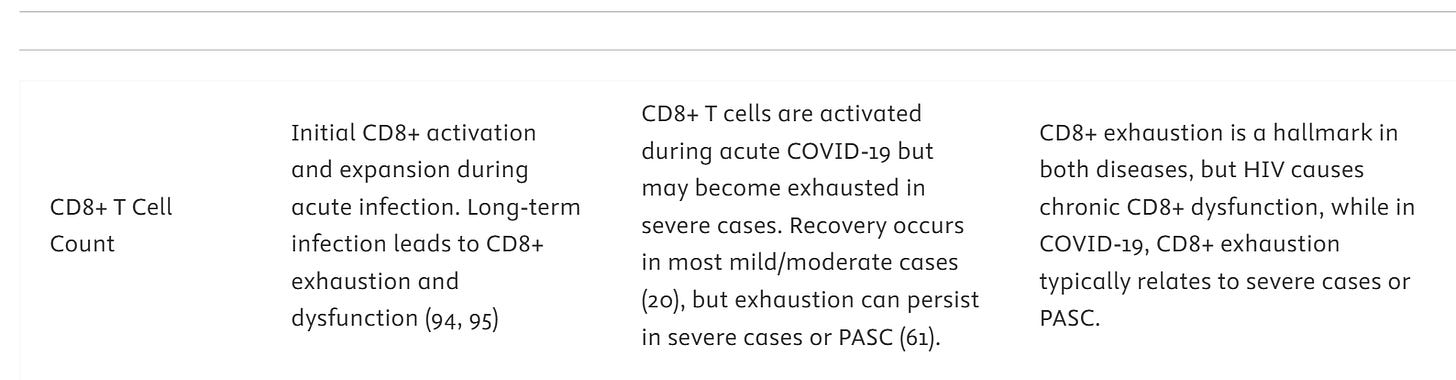
What about CD8 T cells?
Also for HIV, the WHN collective does not understand the immunology. CD8 T cells get activated upon viral infection. They do not understand the difference between “exhaustion” and senescence. They do not understand that CD4 T cells are the main target of HIV, not CD8 T cells. The latter need, however, help from CD4 T cells, also known as helper T cells for that reason. Look at the references the WHN uses:
Also the SARS-CoV-2 part is trying to spell more doom. But what happens is CD8 T cells are activated, some may express markers of “exhaustion” which is not a negative, and indeed recovery occurs in nearly all. PASC is a special case. In these patients there is, for unknown reason which may involve anti-self responses or reduced debris clearance, a increased immune activation. And, if you have more inflammation, you have some more cells expressing the “exhaustion” markers. That is all. (61) is a machine learning study without primary immunological data. It cannot substantiate claims of long-term T cell exhaustion or generalized immune dysfunction, and its use in this context is misleading.
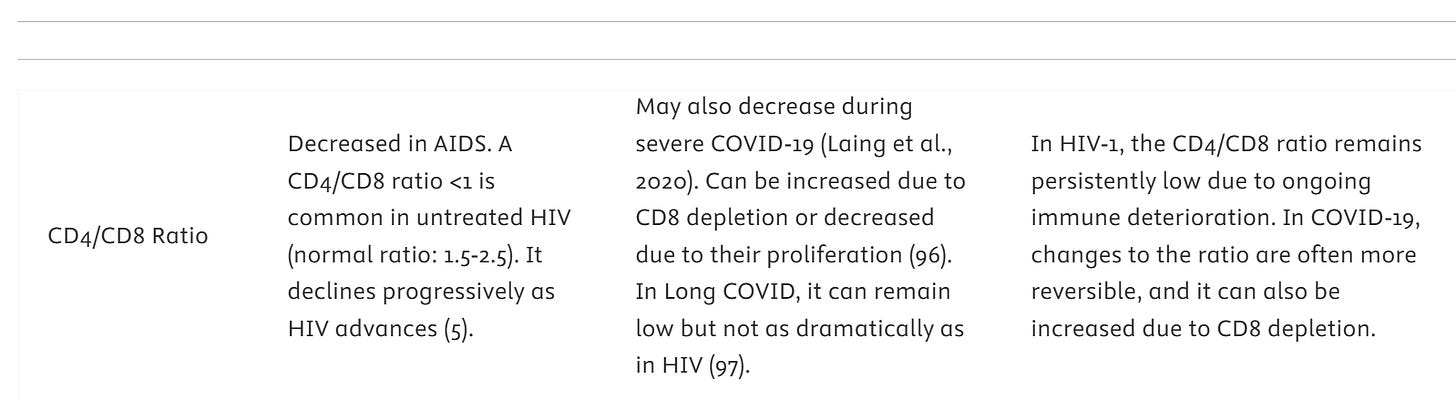
Then you can combine the two CD4 and CD8 T cells and divide them to try and make the same already refuted claims.
In HIV infection, both CD4 and CD8 T cell counts decrease, with CD4 cells being more profoundly depleted, reflecting direct viral infection and destruction.
For SARS-CoV-2/COVID-19, T cell changes are more variable. CD8 counts may transiently decrease or even increase, depending on the intensity of the immune response. These fluctuations are part of the normal immune activation and resolution process. The key point is that, unlike HIV, SARS-CoV-2 does not selectively deplete CD4 T cells nor cause persistent immunodeficiency. Overall, these observations highlight that HIV/AIDS and SARS-CoV-2/COVID-19 are fundamentally different diseases, despite superficial comparisons, and attempts to equate their immune impacts are misleading.
Then other immune activation? Of course, keep in mind, both are viruses, so both will cause immune activation. That again does not mean they are similar!
SARS-CoV-2 infection does not result in chronic viral persistence except in cases of severe immunodeficiency, whether genetic or medication-induced. Reference (19) does not demonstrate viral persistence. Instead, it shows that inflammatory proteins are largely downregulated by three months after symptom onset, with only a small subset (n = 6) exhibiting lingering markers of tissue repair in the lungs. Importantly, this is not specific to SARS-CoV-2, tissue repair is a normal physiological process following many types of infection or injury. Therefore, the WHN collective’s claim that “chronic inflammation may persist” is not supported by the data.
Unique markers?
Again, the WHN collective misrepresents the evidence. There is no viral persistence in SARS-CoV-2 infection. Their citation of (61), a machine learning study, does not demonstrate persistent virus. Claims such as “SARS-CoV-2 triggers a broader, less specific immune dysfunction” are entirely made-up gobbledygook.
Table 1 is equally unconvincing: the WHN collective has not substantiated a single claim. Instead, they have cherry-picked papers from Google searches, including low-impact journals, many of which do not show what the WHN claims, or show phenomena the authors clearly misunderstand.
For example, they state: “T cells expressing co-inhibitory receptors are highly activated in acute COVID-19 disease (38), but become exhausted in Long COVID patients with ME/CFS-like chronic illness (39).” Yes, immune cells are activated during viral infection, but they do not become “exhausted” in the sense implied. The markers cited (LAG3, TIM3, PD-1, TIGIT, CTLA-4) represent physiological negative-feedback mechanisms, not dysfunction, and concern only SARS-CoV-2-specific T cells, very different from HIV, which affects all CD4 T cells.
Reference (39) looked at only 44 Long COVID patients. This is far too small to extrapolate to the general population, analogous to testing a small group of colourblind men and claiming men cannot discriminate reds and greens. What (39) actually shows is heightened immune activation in Long COVID patients, not in those who have recovered from SARS-CoV-2 infection. This stands in stark contrast to HIV/AIDS, where virtually all infected individuals experience CD4 depletion.
“Long-term effects of SARS-CoV-2 infection on immune function sometimes gradually resolve (40) (41, 42), but can persist for months or years (18, 19, 42–44) and might accumulate through multiple infections.” There is a lot to unpack here.
Yes, for many individuals, some symptoms of infection persist, but this is not unique to SARS-CoV-2. Persistence of symptoms has been observed across many pathogens, bacteria, viruses, and parasites, and has long been studied in conditions such as ME/CFS. Risk factors for prolonged symptoms correlate with severity of the initial disease and underlying health conditions, though the exact mechanisms remain unclear.
However, the claim that symptoms accumulate through multiple infections is unsupported by evidence. There is no data showing that repeated SARS-CoV-2 infections progressively worsen long-term immune dysfunction. Were this true, SARS-CoV-2 would be unique among pathogens. While some pathogens show infection-severity interactions, e.g., certain Dengue strains can cause more severe disease upon secondary infection due to antibody-dependent enhancement, HCV can worsen upon reinfection in chronic cases, and HIV-1/HIV-2 interactions can affect each other, these are mechanistically distinct from the claims made here.
“Another relevant immunological observation, cited as common to both diseases, is compromised gut mucosal integrity and microbial translocation, suggested as a mechanism driving chronic inflammation.” While systemic inflammation from any pathogen—including acute viral infections—can transiently affect gut integrity and microbial translocation, this does not make HIV and SARS-CoV-2 comparable. The mechanisms, severity, and long-term consequences differ dramatically between the two infections.
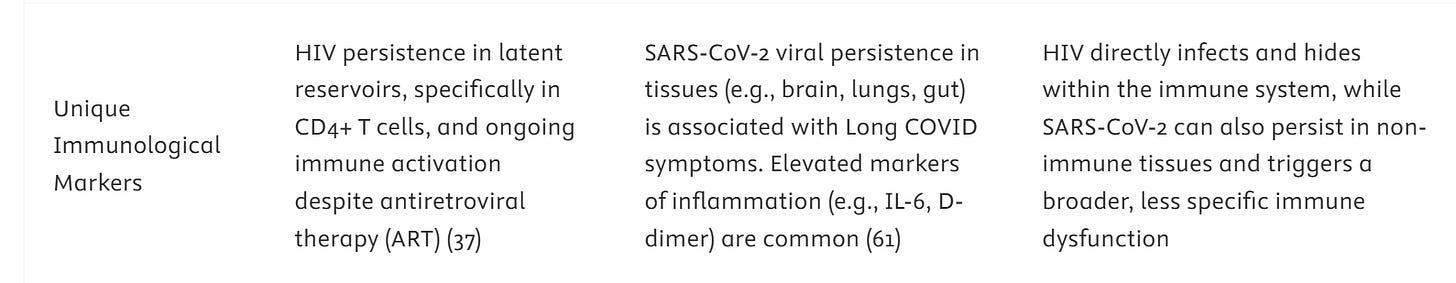
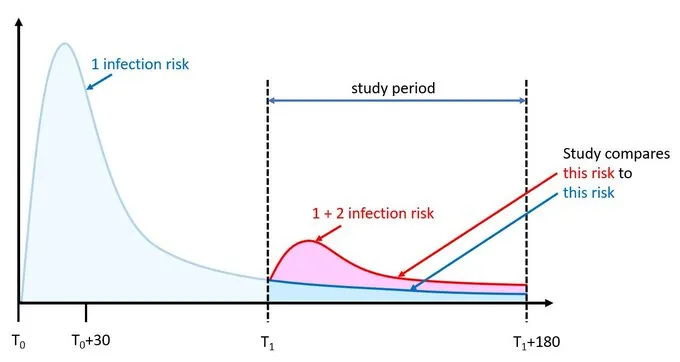
“The WHN collective claim that repeated SARS-CoV-2 infections are associated with a cumulative increase in the risk and severity of Long COVID and PASC (Post-Acute Sequelae of COVID-19) (48–53).”
A closer look at the cited references reveals that this claim is not substantiated:
(48): A retrospective study of 2,511 essential workers categorized participants as having PASC if they reported at least one symptom lasting ≥2 months. Many confounders exist, including the cohort’s prior exposure to World Trade Center disaster stressors. The observed higher number of reinfections in those with PASC does not demonstrate that reinfections cause PASC. Notably, unvaccinated participants were at higher risk, highlighting the protective role of immune memory—directly contradicting the WHN implication.
(49): Reinfection is not mentioned at all; this reference adds no support.
(50): A Veteran Association study in an older, predominantly male cohort. Vaccination appeared not to affect outcomes, and the paper does not assess cumulative risk or severity of Long COVID with reinfection. The study’s authors caution against misinterpretation; WHN citations here are misleading.
(51): Canadian health data with a very small reinfected cohort and numerous confounders; not a robust basis for any claim of cumulative risk.
(52): A narrative review, which by definition does not provide primary data to substantiate cumulative effects.
(53): A review by the WHN collective itself; citing it again does not provide independent evidence.
Conclusion: Despite six references, there is no solid evidence that multiple SARS-CoV-2 infections lead to additive risk or severity of Long COVID. WHN’s repeated claims are not supported by these studies.
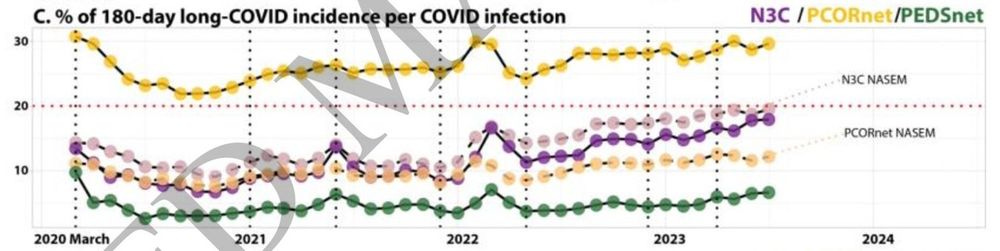
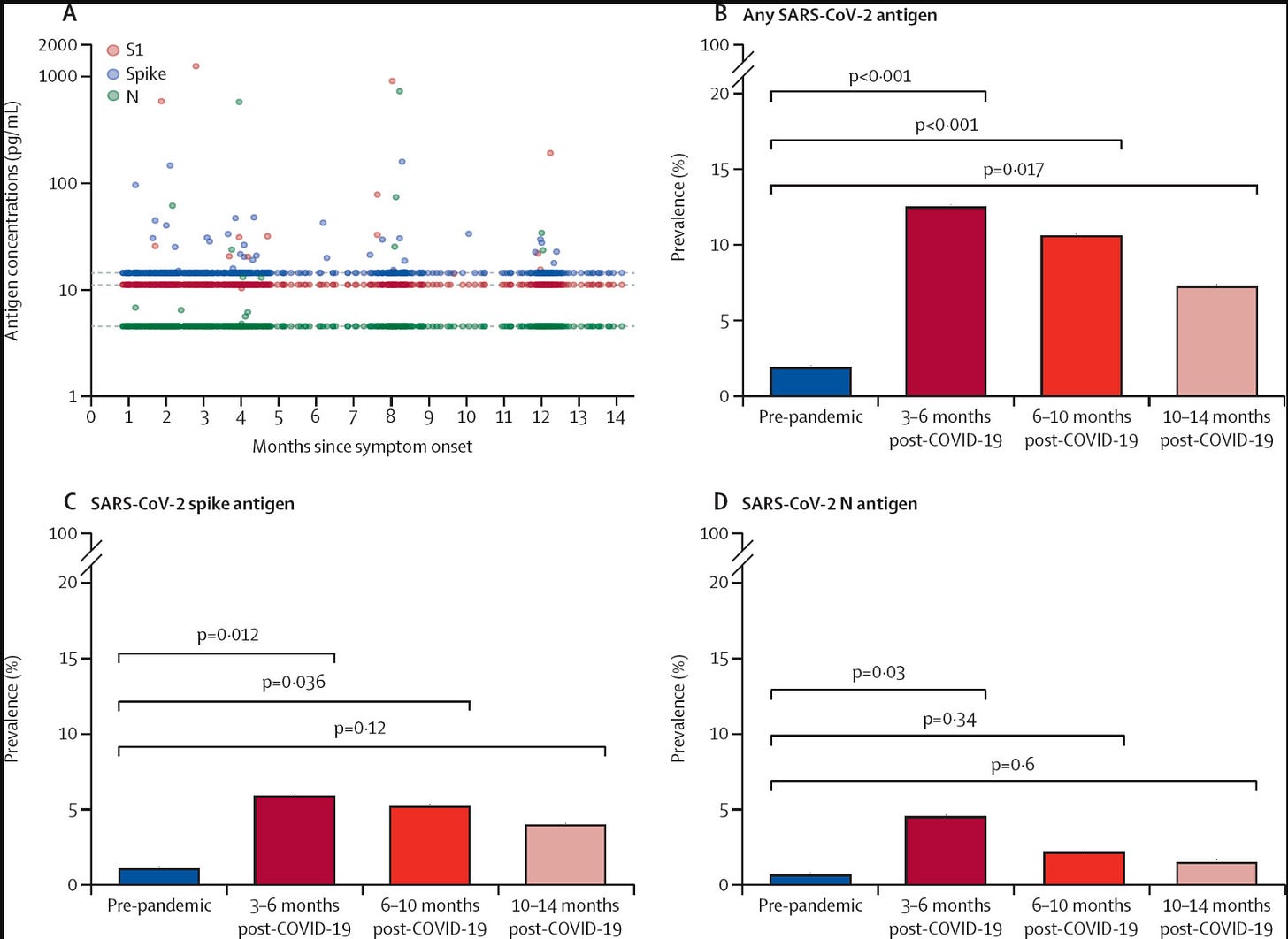
There are indeed well-conducted studies that provide context for the immune response and post-infection symptoms. A novel pathogen, such as SARS-CoV-2 in 2020–2021, can trigger a strong inflammatory response, even without causing severe disease, which correlates with a higher risk of transient long-term symptoms. Consequently, it is expected that the incidence of PASC increased during 2020–2021. However, the exact magnitude is difficult to determine: reported symptoms are often general (e.g., reduced sleep, fatigue) and already prevalent in the general population. Differences in methodology and diagnostic criteria further complicate incidence and prevalence estimates, even within the same society.
In the post-pandemic period, secondary symptoms appear to decline. Reports from 2022-2023 indicate a reduction in long-term symptom burden, and by 2023-2024, prevalence is largely consistent with background levels. These trends align with observations following previous pandemics (see also my BlueSky thread). This pattern demonstrates that there is no cumulative effect from repeated SARS-CoV-2 infections and that immune memory provides protection. That said, as with many infections, some residual long-term effects remain in a minority of individuals. Overall population health has continued to improve, reflected in rising life expectancy, further underscoring that post-pandemic outcomes are consistent with expected patterns rather than evidence of widespread, accumulating immune dysfunction.
The WHN collective largely ignores historical data and established patterns, instead relying on fear and “what if” scenarios. For example, they claim:
“Immune system dysregulation is associated with other types of damage and symptoms found in Long COVID (39, 54–60). This indicates a potential parallel (61) in which the immune system may experience gradual deterioration or increased dysregulation with successive infections.”
This assertion is nonsense. Reference (61) is a machine learning paper and provides no primary evidence for such claims. The remaining references appear to have been selected based on titles rather than careful reading or comprehension.
(39): Previously discussed, this study shows heightened immune activation in Long COVID patients, not in recovered individuals. It cannot be generalized to all SARS-CoV-2 infections. Unlike HIV/AIDS, where all infected individuals experience CD4 depletion, here the effect is limited and specific.
(54): A JLB review paper; no primary data. It proposes hypotheses, such as potential neutrophil alterations, but provides no evidence of gradual immune deterioration.
(55): A frequently misused study. “Dysregulation” here refers only to a prolonged immune response in Long COVID patients, which is not SARS-CoV-2-specific and occurs with other post-infectious syndromes.
(56): Similar to reference (29), this examines microbiota dysbiosis, which is a temporal effect caused by inflammation and immunosurveillance. Again, this is physiological and not SARS-CoV-2-specific.
(57): Immune profiling in Long COVID patients shows prolonged immune activation, but not in SARS-CoV-2-infected controls. Extrapolating this to the general population is misleading. It is akin to observing injuries among hospitalized skiers and concluding that all skiers will suffer fractures.
(58): An allergy study interpreted as showing a Th2 response. In reality, intracellular pathogens, including viruses, predominantly induce a Th1 response. The paper is prone to p-hacking, splitting data into ever-smaller subgroups until apparent differences emerge, which are unlikely to be meaningful. A more detailed explanation on my BlueSky account.
(59): Reviews showing microbiota changes post-infection; again, not SARS-CoV-2-specific.
(60): Scientific Reports study of unvaccinated Long COVID patients. Extrapolating findings from a small, selective group to the entire population is invalid—analogous to surveying ten marathon runners and concluding that everyone enjoys running 42 km.
The WHN collective repeatedly overstates limited observations, misinterprets studies, and extrapolates from unrepresentative cohorts, all while ignoring broader historical and epidemiological context.
The WHN collective boldly claims:
“A common outcome in both HIV and SARS-CoV-2 infections is increased vulnerability to infections.”
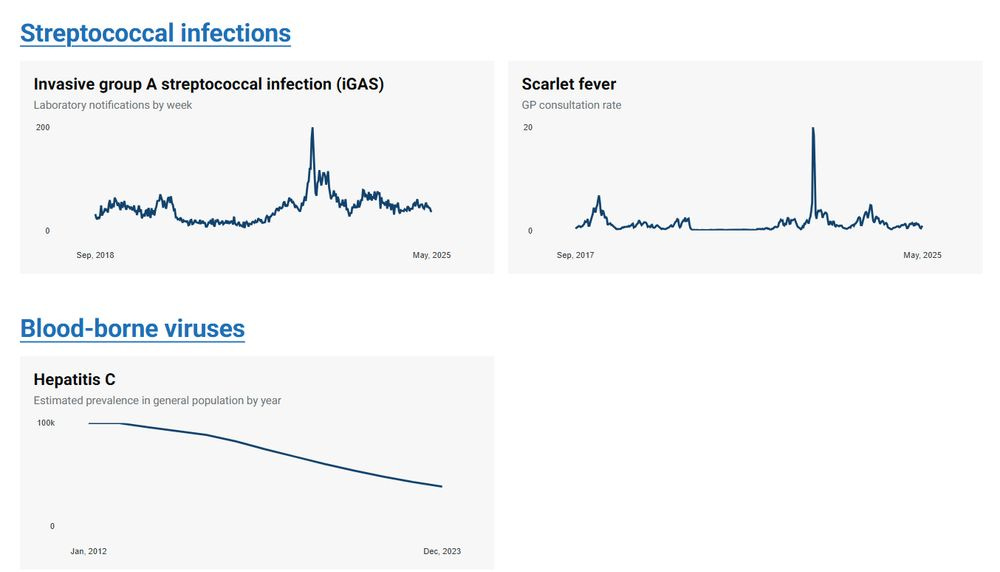
This is misleading. In HIV, once CD4 T cell numbers are sufficiently depleted, clinical symptoms, termed AIDS, manifest as opportunistic infections such as oral thrush, skin rashes, and lesions. This is a direct consequence of immune collapse. By contrast, coronavirus infections do not produce this outcome. Presenting this as a fact without supporting data reveals the WHN collective’s anti-science bias. Observing annual viral infection patterns requires no advanced science: epidemics come and go, waves end, and population immunity is clearly effective. Cataloguing major infections over time shows a largely stable landscape. Yes, with thousands of pathogens, some fluctuations occur—new strains emerge, multi-year cycles repeat, antibiotic resistance rises, or vaccination coverage drops, but cherry-picking these exceptions and presenting them as evidence of “immunodeficiency” is scientifically unsound. Yet this is exactly what the WHN CovidDoomers attempt to convince others of.
This overview, compiled by UKHSA, is comprehensive and unselected, and it completely undermines the WHN collective’s claim of “immunodeficiency.” Nowhere is it shown how SARS-CoV-2 could plausibly cause such a systemic immune collapse. While B and T cell numbers may transiently decline in the blood during severe cases, numerous studies repeatedly demonstrate full recovery afterward. Yet, despite this overwhelming evidence, the WHN collective continues to propagate the same false claims.
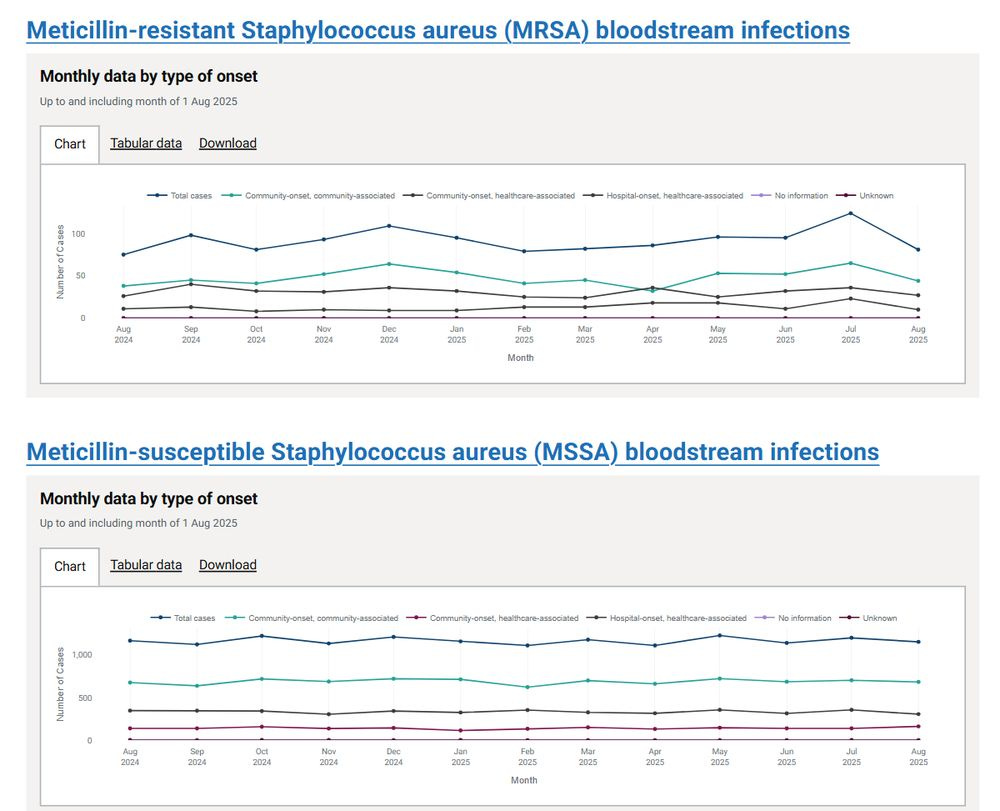
Indeed, the WHN collective goes further, claiming: “Immune function after COVID-19 infections is characterized by increased risks of infections (50, 62–65), including a greater risk of antibiotic-resistant infections compared to influenza (66), and emerging evidence for opportunistic, AIDS-defining (67) infections like various mycoses (68–71), Pneumocystis jirovecii (72), tuberculosis (73), cryptococcosis (74, 75), cryptosporidiosis (76), methicillin-resistant Staphylococcus aureus (MRSA) (66), and others (77, 78), likely also several types of cancer (79–85). Immunodeficiency and other long-term COVID effects such as mitochondrial (86) and DNA damage (87, 88) provide potential mechanistic explanations for increased risk of cancer onset and/or progression (79–85).” Let’s examine what these references actually show.
(50) Is a own WHN opinion work, which is not evidence
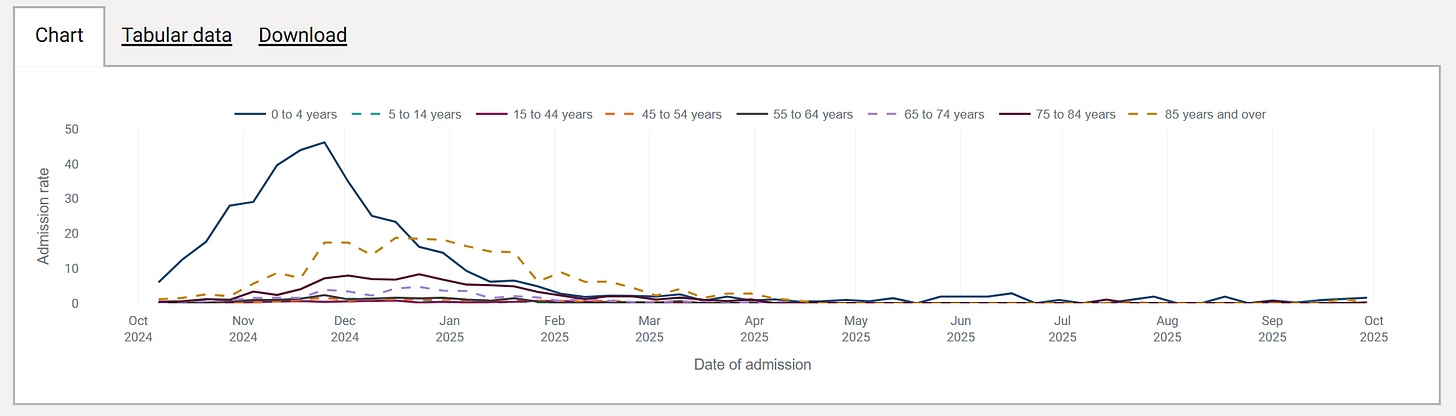
(62) The RSV association study cited by the WHN collective focused only on children aged 0–5 years. A larger RSV wave observed after the relaxation of anti-pandemic measures is not evidence of “immunodeficiency.” Why? Because if COVID-19 caused widespread immune dysfunction, such increases would continue indefinitely, which they did not. The more plausible explanation is an infection pause / immunity gap: during the pandemic, children were born or remained unexposed to RSV due to reduced social contacts, and toddlers did not encounter the virus at the usual time to build robust immune memory. The result was a temporarily larger RSV wave, but limited to this age group, with no comparable effect in teenagers or adults. Average RSV waves have since returned to normal, showing no evidence of systemic immunodeficiency.
This explanation is further supported by recent studies showing that antibody levels in this age group lagged during the COVID-19 measures, particularly against RSV and Streptococcus pyogenes (GAS), the two pathogens that did indeed show temporarily higher incidence and clinical effects.
Does this phenomenon occur in adults? Yes, potentially, but adults typically already have high levels of immunity, making reductions slower and less clinically significant. Moreover, when a virus is absent for several generations and/or mutates enough to partially evade antibodies, as is common with influenza, more severe illness can occur once it is re-encountered. This is normal immunological behaviour, not evidence of SARS-CoV-2–induced “immunodeficiency.”
(63) Another Veterans Association study. This cohort consisted of older (60+) white men with multiple underlying health conditions, making it not representative of the general population. What the authors actually show is that SARS-CoV-2 infection adds an incremental burden on top of pre-existing conditions. It does not demonstrate immunodeficiency or a general increase in infection susceptibility. Using this study to support such an outlandish claim is therefore inappropriate.
(64) A Frontiers review on influenza infection. Again, this is not evidence for SARS-CoV-2–induced immunodeficiency; it appears the WHN collective merely Googled titles without assessing the content, then treated a review of a different virus as “primary evidence.”
(65) 😂🤣 Seriously? A conspiracy piece from the WHN’s own webpage. This is not scientific evidence and should not be cited in any serious discussion.
(66) It is true that during acute infection, secondary infections can occur. This is well-known for many pathogens, including influenza, and occurs less frequently with SARS-CoV-2. This does not indicate immunodeficiency. MRSA infection rates are stable, and comparing infections in a pandemic cohort (March 1, 2020–September 30, 2022) with endemic infections is misleading; it is not a fair comparison.
(67) The WHN authors cite the MSD AIDS Manual. This source contains no primary data on SARS-CoV-2 or COVID-19, demonstrating their reliance on general reference material rather than rigorous scientific studies. It highlights a fundamental misunderstanding of immunology.
(68) Many cited references are reviews without primary data. Reports of mucormycosis, aspergillosis, and candidiasis in COVID-19 patients almost exclusively involve individuals who were steroid-treated, ventilated, or diabetic, all well-known risk factors for opportunistic infections. The WHN authors label these patients as “immunocompromised,” but there is no evidence that SARS-CoV-2 causes generalized immunodeficiency.
(69) P133 …. a conference poster. This shows the WHN collective is scraping the bottom of the barrel. They Google keywords, select what suits their narrative, and pretend to have reviewed the literature thoroughly. Their lack of expertise in immunology and virology is evident.
(70) A review linking corticosteroid use with fungal infections during or shortly after SARS-CoV-2 infection. Evidence for WHN’s claim: 0.
(71) Single case of a diabetic patient with a fungal infection. Evidence: 0.
(72) Six patients, all on steroids with fungal infections. Evidence: 0.
(73) Study in Turkey, not PubMed-listed. Many had prior TB, steroid use, or other confounders. Evidence: 0.
(76) Claims linking azithromycin, hydroxychloroquine, and ivermectin to Cryptosporidium infection. Evidence: 0.
(77–78) Case studies, patients on steroids or antibiotics. Evidence: 0.
(79–80-81) Reviews or opinions. Evidence: 0.
(82) Mendelian randomization study attempting to find genetic associations. No causal evidence for immunodeficiency. Evidence: 0.
(83-84–85) Patients with pre-existing cancer or immune disorders. WHN misrepresents correlation as causation. Evidence: 0.
(86) Review discussing potential mitochondrial involvement in infection or long-term symptoms. Evidence: 0.
(87–88) Papers on SARS-CoV-2 effects in cell lines (DDR, DNA machinery). Nothing about systemic immunodeficiency. Evidence: 0.
In short: one long sentence, 19 references, and none substantiate the claim of population-wide immunodeficiency or increased infection risk due to SARS-CoV-2. Many references are reviews, case reports, or unrelated papers. Some even deal with influenza, steroid use, or pre-existing conditions, not SARS-CoV-2.
Yet the WHN collective repeatedly hammers this false narrative, using the same misrepresented references, pretending that increased infection risk is proven. It is not. It is misleading, anti-scientific, and relies on readers not verifying the sources.
The WHN collective continues:
“Some SARS-CoV-2 reinfected patients can experience less severe symptoms in the acute phase, however meta-analyses point to similar acute severity of reinfections (89).”
Translated: they want you to believe that SARS-CoV-2 is uniquely incapable of inducing immune memory, so that after a first infection, all SARS-CoV-2-specific antibodies and T cells suddenly fail, leaving you fully vulnerable to the next infection. This is completely bizarre and unsupported. Reference (89) is an MDPI journal article based on literature searches. Importantly, the literature is biased: asymptomatic or very mild infections are often underrepresented, because they rarely get reported or published. These gaps are exploited by anti-vaccine activists and COVID-Doomers to inflate the perceived risk of reinfection or the supposed “failure” of immune memory.
“Acute severity of SARS-CoV-2 reinfections can also be enhanced, especially in individuals with increased exposure to reinfections (24).” This reference (24) is the very same small study already discussed: only 33 subjects with recurrent, symptomatic infection. Importantly, the cohort is highly selective, it only includes reinfected individuals who were symptomatic. It is not representative of the general population and therefore cannot substantiate a broad claim about reinfections causing increased severity. “with a relatively high risk of hospitalization among the reinfected cases (91).”
Reference (91) is based on a selective literature search (SISO approach). The observed higher hospitalization risk reflects older or medically vulnerable individuals, not a general property of SARS-CoV-2 reinfections. Any infection in these populations carries increased risk, this is expected and not unique to COVID-19. Focusing on such cohorts naturally produces the observed outcome.
“Regardless of the severity of acute disease, the long term symptoms, organ damage and health risks increase with each SARS-CoV-2 reinfection (50, 52). SARS-CoV-2 reinfections are increasingly common post-Omicron (92).”
In reality, reference (50) (the VA study) does not assess cumulative long-term effects of reinfections, and the Canadian Health data (52) is not robust scientific evidence. Reference (92) reflects a misunderstanding of viral evolution: new variants are naturally selected for increased infectivity, just as with influenza, RSV, OC43, NL63, and many other viruses. Yes, reinfections will occur, but this is expected immunology, not evidence of compounding damage. Antibodies wane over time, and new variants may partially evade existing immunity, but infection or vaccination significantly reduces disease severity. The statement from (92): “Our analysis suggests that a single infection from SARS-CoV-2 may not generate the protective immunity required to defend against reinfections from emerging Omicron lineages” is trivial and expected, not alarming or evidence of enhanced long-term risk.
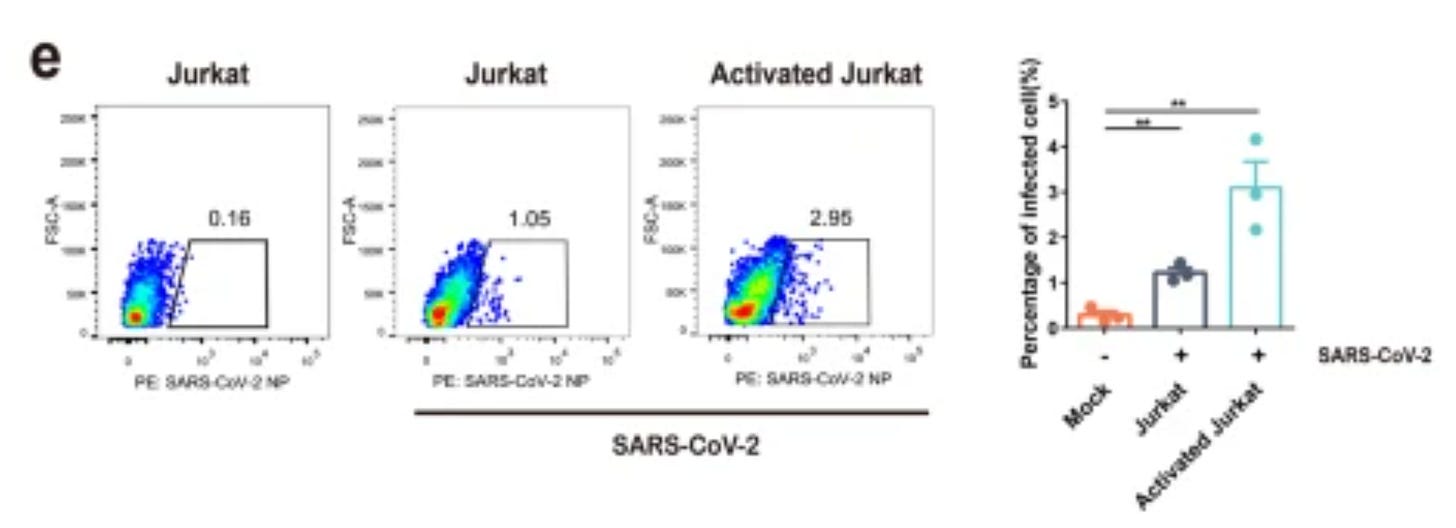
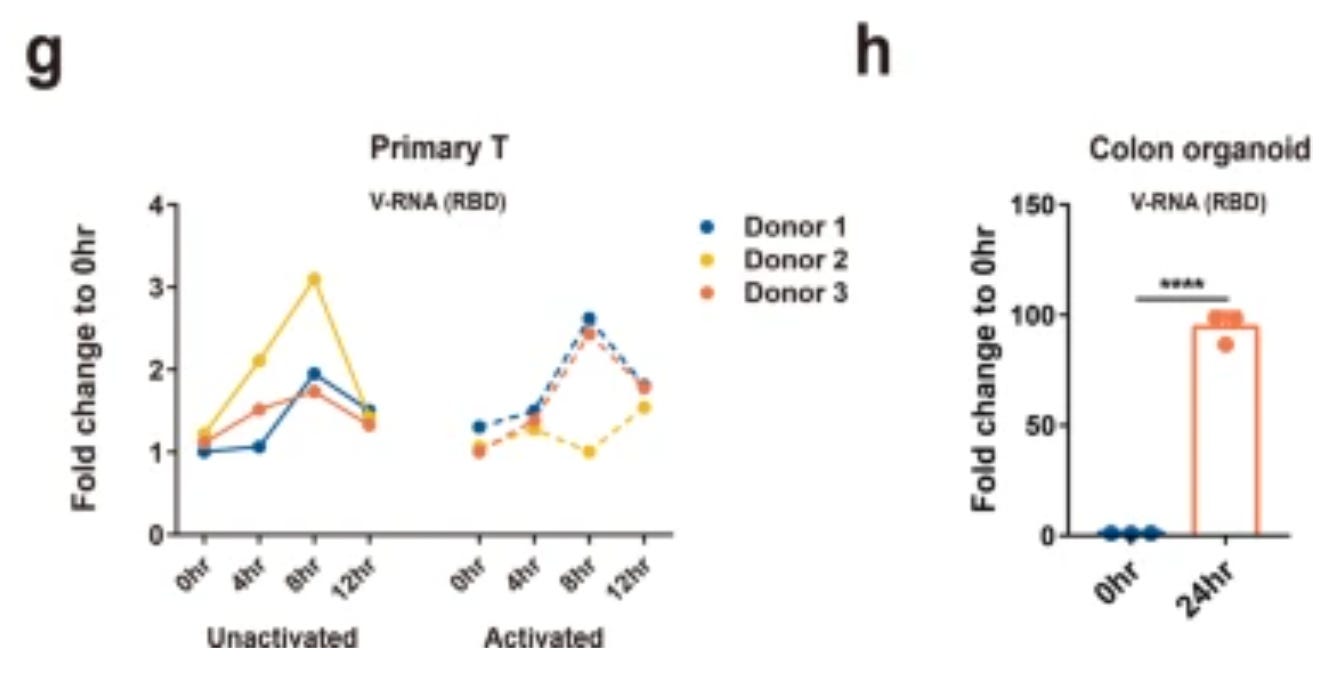
“While SARS-CoV-2 can directly infect T-lymphocytes (99, 100), this is likely not the primary mechanism of immune dysfunction.” Indeed, first of all because there is no immune dysfunction. Secondly, infection of T cells seems unproductive, very low level if it even happens at all. Many have checked and not found infected T cells.
(99) Some binding to the outside of the cells. You can find some RNA (which is not the virus), but no productive infection. Viral entry is shown in a cell line: 293T, known for its susceptibility to infection, and good use as a packaging line.
(100) Same here: low levels,
and not productive (viral level does not increase over time).
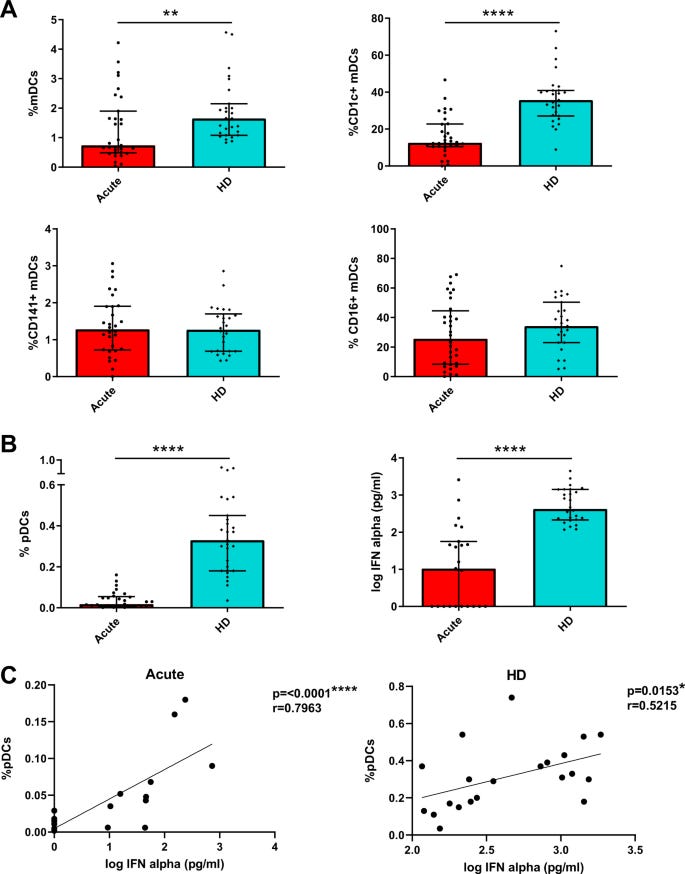
The WHN collective continues to inflate fears to support their idea of “immunodeficiency”: “Instead, COVID-19 immunopathology is diverse, involving reductions in both CD4 and CD8 T cells, their functional exhaustion and premature senescence (101) (39), dendritic cell deficiencies (40), neutrophilic granulocyte dysfunction (102), impaired B-cell function (103), gastrointestinal dysbiosis (59), endotheliopathy (104, 105), reprogramming (21), autoimmunity (106, 107) (108) (30) and pathological clotting (109) (110) (111).”
In reality, none of this substantiates general immunodeficiency. We have already addressed “exhaustion”, it is physiological, part of normal immune regulation, and not evidence of permanent dysfunction. Other claims, from dendritic cell or neutrophil alterations to autoimmunity, dysbiosis, or endothelial changes, are cherry-picked, misinterpreted, or observed only in small or highly specific cohorts (e.g., hospitalized or LongCOVID patients). The WHN collective demonstrates a fundamental lack of understanding of immunology, conflating normal immune responses, transient changes, and pathological states.
(39) has been addressed earlier: it demonstrates heightened immune activation, not universal exhaustion, and only in LongCOVID patients—not in those who recovered normally. This is very different from HIV/AIDS, where all infected individuals experience CD4 depletion. Yes, one could loosely call it “dysregulation,” but only in the broad sense of deviation from homeostasis, not as a general immune collapse.
(101) concerns hospitalized patients with severe COVID-19, mostly elderly. What do older adults naturally have? Higher proportions of senescent immune cells, which explains many of the findings without implying SARS-CoV-2 causes generalized premature senescence.
(40) claiming dendritic cell deficiencies, this reflects a misunderstanding between absolute numbers and relative proportions. Confusing percentages with counts is a basic error; those who misinterpret it have no place claiming broad immunological dysfunction.
(102) reports differences in neutrophils. Could this contribute to LongCOVID in some patients? Possibly. But there is absolutely no evidence that these changes are caused directly by SARS-CoV-2 infection. Level of evidence for general immunodeficiency: 0.
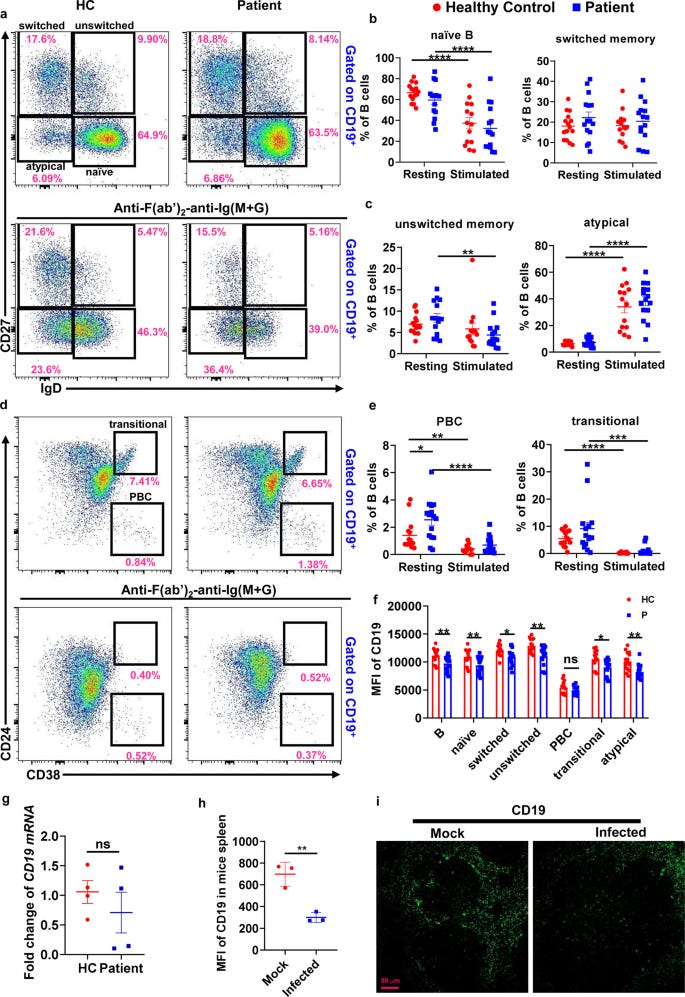
(103) is a bioinformatics analysis artifact. The observed downregulation of certain receptors simply reflects normal activation of B cells. The claim that a small proportion of B cells “disappear” is misleading, it is merely a technical observation in single-cell RNA sequencing. Again, level of evidence for immunodeficiency: 0.
Importantly, the differences reported are predominantly between resting and activated cells, not between COVID-19 patients and uninfected controls, further undercutting any claims of SARS-CoV-2-induced immunodeficiency.
(59) reports alterations in the microbiota following infection. This is a normal physiological response and is not specific to SARS-CoV-2. Once again, this is a review and provides no primary data to substantiate the WHN collective’s claims.
(104) highlights that SARS-CoV-2, like HCoV-NL63, uses ACE2, which is expressed on endothelial cells. Infection can alter gene expression in these cells, as shown in the hBMEC cell line, but this is a standard cellular response to viral infection and does not indicate broad immunodeficiency.
(105) emphasizes that infections by viruses, bacteria, or parasites always induce changes in cellular gene expression. This is expected and well-understood; the level of alarm the WHN collective suggests is entirely unjustified.
(106) is an opinion and overview, not primary research. Its use to claim SARS-CoV-2-specific immunodeficiency is unsupported. Level of evidence: 0.
(107) focuses only on PASC patients. While the questionnaire included vaccination status, this was not analyzed. Findings fall into the category of “may” or “can”—as with any infection. Level of SARS-CoV-2-specific “magic”: 0.
(108) notes that prolonged or severe inflammation can increase the risk of anti-self responses. This is a general physiological phenomenon, not unique to SARS-CoV-2. Level of SARS-CoV-2-specific magic: 0.
(109) is an opinion/review. Yes, inflammatory or clotting events can occur, but this is not evidence of SARS-CoV-2-specific immunodeficiency. Level: 0.
(110) presents more opinions. Again, immune events happen with all infections, not specifically SARS-CoV-2. Level: 0.
(111) documents thromboses. Once immune memory is established and viral replication is controlled, the risk is very low. SARS-CoV-2-specific “magic”: 0.
And on repeat again: “Additionally, in Omicron lineages there is enhanced inhibition of MHC-I expression (14) and suppression of innate immunity (15). As a highly cytotoxic virus, SARS-CoV-2 can also promote lymphocytopenia by direct damage to secondary lymphoid organs (112, 113).“
We have dealt with the overinterpretation and lack of understanding regarding MHC. Like influenza and many viruses, SARS-CoV-2 is cytotoxic: it kills its host cell.
(112) claims SARS-CoV-2 “decimates secondary lymphoid organs”, scary wording! In reality, the study examined 18 deceased COVID-19 patients, all of whom died within three days of admission to the First Pneumonia Ward of Huoshenshan Hospital (Feb–Apr 2020) from ARDS, a severe, life-threatening condition.
Such destruction of lymphoid tissue can occur in any severe systemic infection and is part of the extreme inflammatory response, now often managed with treatments like dexamethasone. It is not representative of the general population. Extrapolating these observations to suggest widespread immune devastation is misleading and alarmist, clearly intended to scare rather than inform.
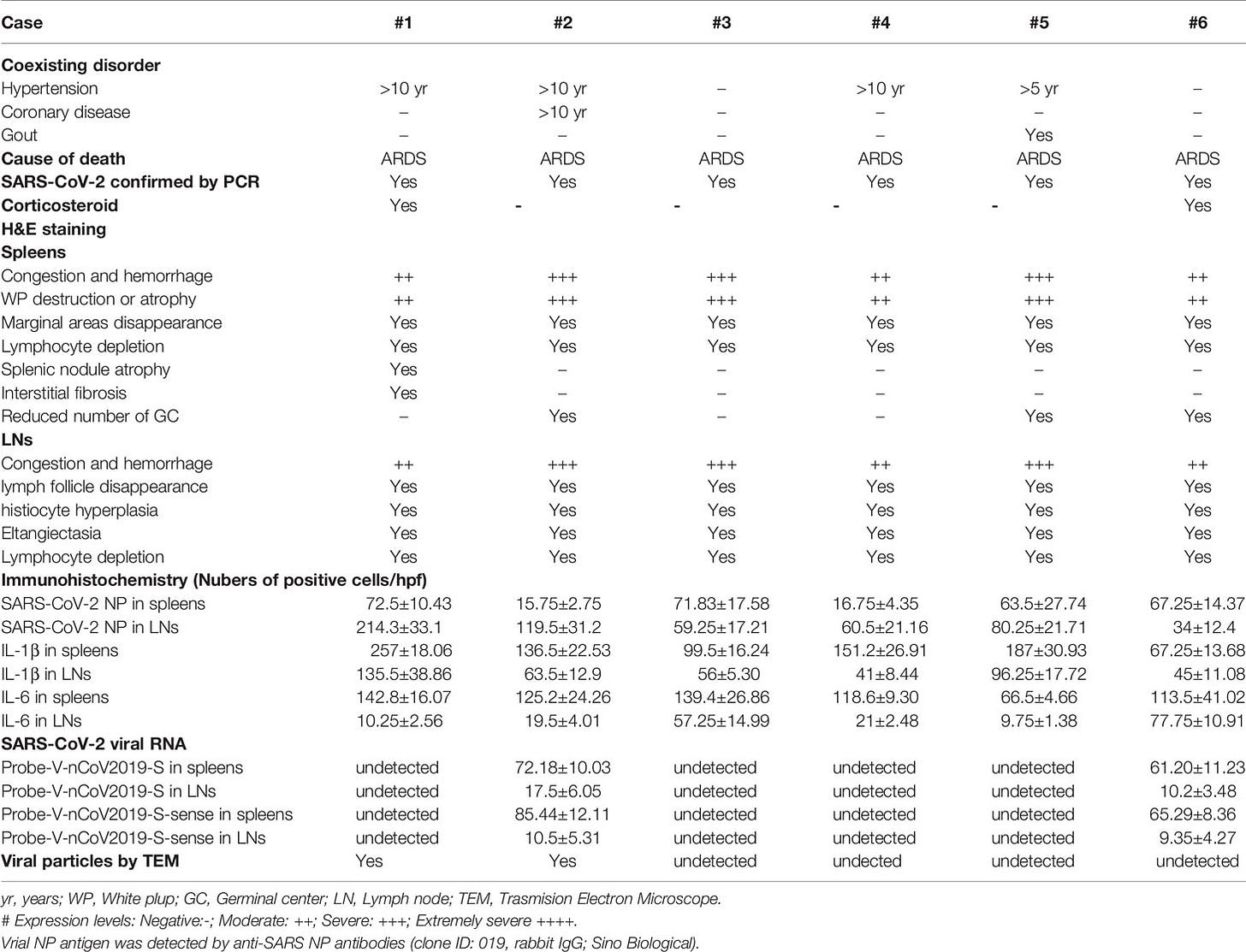
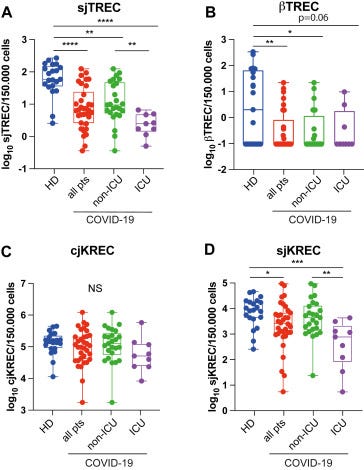
(113) examines the thymus, the “school” for T cells. Thymic activity naturally declines from the twenties and is minimal in older age. Severe illness or stress can cause temporary reductions in thymic output, which is exactly what this study observed—particularly in severe ICU COVID-19 cases.
This is a physiological response to severe illness, not a SARS-CoV-2–specific effect. Far from supporting the WHN claims of widespread immune damage, it actually undermines their assertions.
The WHN collective once again attempts a summary to reinforce their misleading narrative. They reluctantly acknowledge that similar immune phenomena occur during influenza and many other infections (114). Yet they propagate disinformation by claiming “the rapid waning of acquired immunity in the post-Omicron era”, deliberately implying that immunity is quickly lost. This is false. Waning of neutralising antibodies is physiological, expected for all pathogens, and does not mean loss of protection, since B and T cell memory persists and safeguards against disease and severe outcomes (115).
In reality, when robust T and B cell memory exists, the immune system rapidly deploys these defences upon re-exposure. It can also generate new T cells and antibodies against variant-specific epitopes, prioritizing conserved sites. This is not alarming; it is adaptive immune strategy at work, ensuring rapid control and clearance of reinfections.
In this section, the WHN collective demonstrates a clear lack of scientific rigor. They appear to have Googled papers selectively, interpreting them to fit a biased narrative rather than reading and understanding the actual data. As a result, they make sweeping claims without evidence, and in many cases, the cited studies either report general immune phenomena or directly contradict the assertions. Their repeated comparison of COVID-19 with HIV/AIDS is particularly misleading and scientifically incorrect.
In contrast, a number of high-quality studies demonstrate that immune cell numbers recover after acute COVID-19, that lymphopenia is largely restricted to severe cases, and that the majority of individuals mount robust and durable immune responses post-infection. A curated list of these papers can be found under Post-COVID-19 immune competence.
In this section, the WHN collective made a mess. They show they Googled some papers based on their biased view. They did not read those papers, nor understood them. They make sweeping claims, but provide no evidence for them. What they provide does often show general issues or contradicts their claims. And that comparison between COVID-19 and AIDS, that was nowhere. Because it is very wrong. A small collection of reference clearly showing immune competence after COVID-19 can be found here.
Interlude: Understanding Inflammation and Long-Term Effects
Inflammation is a tightly regulated, potentially dangerous process, initiated only when strictly necessary. All immune activation operates through a system of checks and balances, making the immune response highly complex. Each step requires multiple signals and regulatory mechanisms.
The facts: Long-term effects can follow many types of infections. Known risk factors include sex and the severity of the immune response. This indicates that post-infection symptoms are not necessarily pathogen-specific, but are largely driven by immune factors released during inflammation. Which specific factors act on which cells remains largely unknown. Clearance of pathogens and damaged cells, as well as initiation and regulation of tissue repair, is also performed by immune cells. Several hypotheses attempt to explain long-term symptoms, but none are strongly supported by robust data. Complicating this further, poorly defined diagnostic criteria and the high prevalence of overlapping symptoms in the general population dilute signals in clinical studies.
Each inflammatory response carries a small risk of generating self-directed immune activity. This occurs regularly, is generally non-pathogenic, and usually resolves after the infection clears. Over a lifetime, low-level auto-antibodies accumulate without causing disease in most individuals.
Evidence in subjects with long-term symptoms shows:
Increased immune activation, indicated by elevated proportions of effector/memory T cells.
Often higher levels of anti-SARS-CoV-2 S protein antibodies.
Expression of regulatory molecules such as Tim-3, LAG-3, PD-1, CTLA-4, and TIGIT, often mischaracterized as markers of “exhaustion.” These molecules are part of normal negative-feedback mechanisms to limit tissue damage, not indicators of a “tired” immune system.
Hypotheses for long-term effects after SARS-CoV-2 infection
Immune exhaustion: No evidence supports this.
Immune damage: No evidence supports this.
Immune dysregulation: Refers to prolonged immune activation. Evidence for increased activation is strong, but it remains unclear whether this is a cause or consequence of symptoms. Trials using immune inhibitors (e.g., corticosteroids) have not consistently reduced symptoms, though they are effective during acute severe infection.
Failure to clear debris: Viral RNA or protein fragments have been observed, but also in individuals without long-term symptoms. Some studies show altered neutrophil and NK cell activity, but the causal link to symptoms is weak and unclear.
Viral persistence: Although viral debris may persist, no replication-competent virus has been detected at late time points, except in severely immunocompromised patients. Viral persistence does not correlate with long-term symptoms, and antiviral trials have shown no consistent clinical benefit. Evidence is very weak.
Autoimmune responses: Some auto-antibodies have been identified, but overall correlations with symptoms are inconsistent. Corticosteroid treatment generally does not reduce symptoms. In specific cases, certain antibodies can transfer symptoms to mice, suggesting a possible contributing role in some patients.
Viral reactivation (e.g., herpesviruses): Reactivation occurs in both symptomatic and asymptomatic individuals. Antivirals have not demonstrated clinical benefit. Evidence is very low.
Tissue reservoirs and long-term persistence of viral effects
This section opens with a bold claim:
“Both HIV-1 and SARS-CoV-2 persist in tissue reservoirs, contributing to chronic immune dysregulation and systemic damage. HIV-1 integrates into the host genome (37), making eradication nearly impossible, while SARS-CoV-2, though not integrating into DNA, has been detected in tissues such as the brain, heart, lymphoid organs, gastrointestinal tract, and lungs long after infection (116, 119-123).”
Let’s unpack this. HIV-1: Yes. HIV-1 forms true tissue reservoirs because it integrates into the host genome, particularly in CD4⁺ T cells and macrophages, making eradication extremely difficult. This is well established.
SARS-CoV-2: No. There is no evidence of persistent, replication-competent virus in tissues in the general population. Detection of viral RNA or proteins in some tissues has been reported, but this does not equate to reservoirs of active virus.
(116) : A pre-print, not peer-reviewed. The study reports higher tracer levels, which the authors interpret as T cell activity. However, these signals could come from multiple cell types and reflect immune activation, not viral presence! There is no data confirming replication-competent SARS-CoV-2 in tissue.
(119) The title mentions “persistence” and “association,” but this is a commentary, not primary research. There are no data on viral persistence. This shows that the WHN collective relied on title searches rather than critically reading the paper.
(120) This is a primary research paper. Do they find persistent SARS-CoV-2? No. The study reports protein fragments, not intact, replication-competent virus. Much of the experimental work is in mice, and the images used by the WHN were manipulated to exaggerate their point. There is no evidence of persistent infection in humans from this study.
(121) This paper reports detection of antigen, not replicating virus, and only during acute infection. The study is from April 2020, when there was no immune memory in the population. It also shows that antigen detection is more frequent in hospitalized or severe cases, which aligns with a higher viral burden during acute infection. This is normal biology, not evidence of chronic persistence.
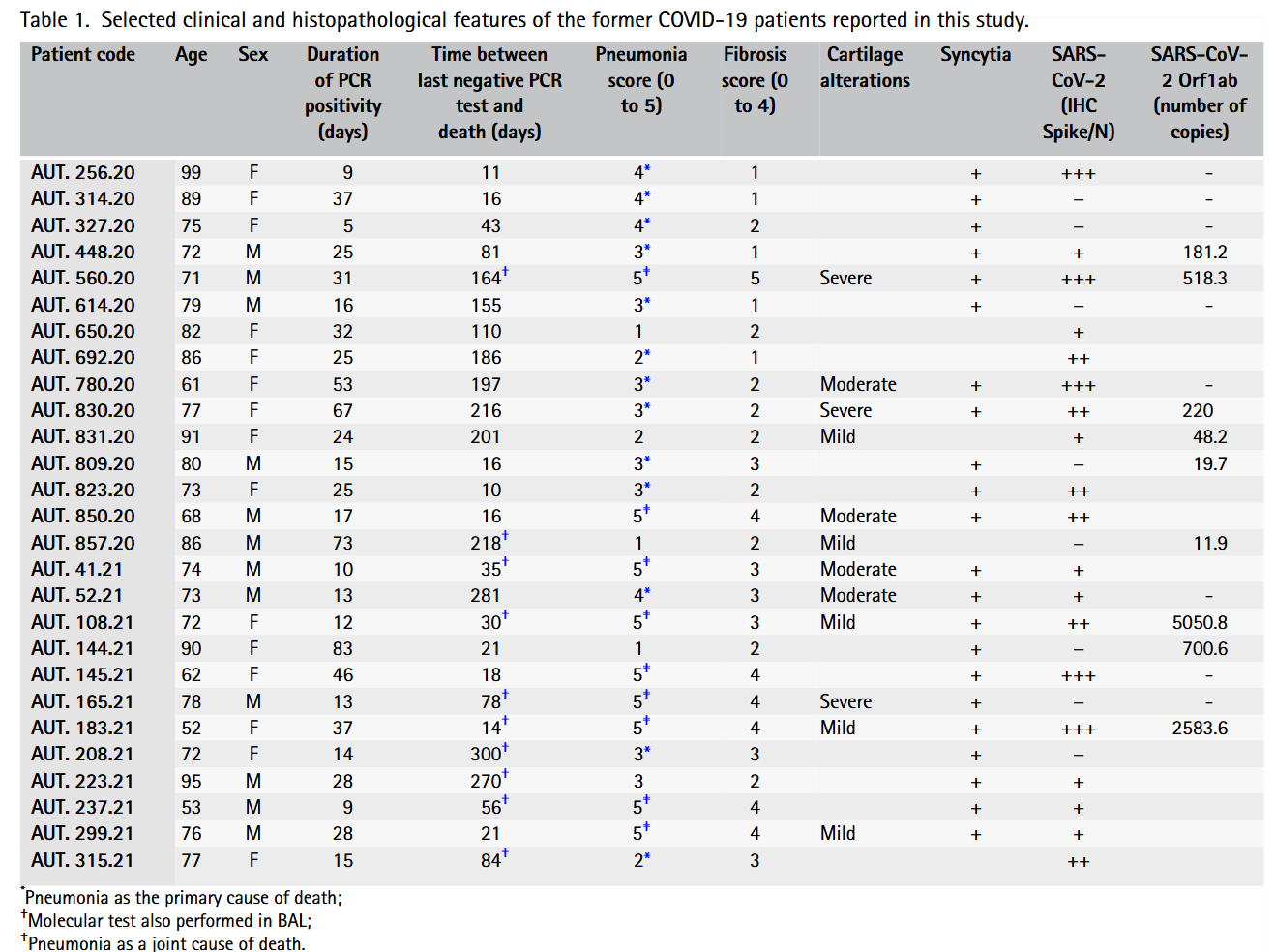
(122) The title mentions “persistence,” but this study is based on autopsies of patients who died from COVID-19. These individuals failed to control the infection, which is not representative of the general population. Extrapolating these findings to all SARS-CoV-2 infections is scientifically invalid.
(123) The title also mentions “persistence,” but this is a review, containing no primary data on viral reservoirs.
Conclusion: These references do not support the WHN claim that SARS-CoV-2 establishes tissue reservoirs similar to HIV. The WHN collective is relying on the word “persistence” in titles rather than actual evidence. There is no peer-reviewed data showing chronic SARS-CoV-2 infection in otherwise healthy individuals.
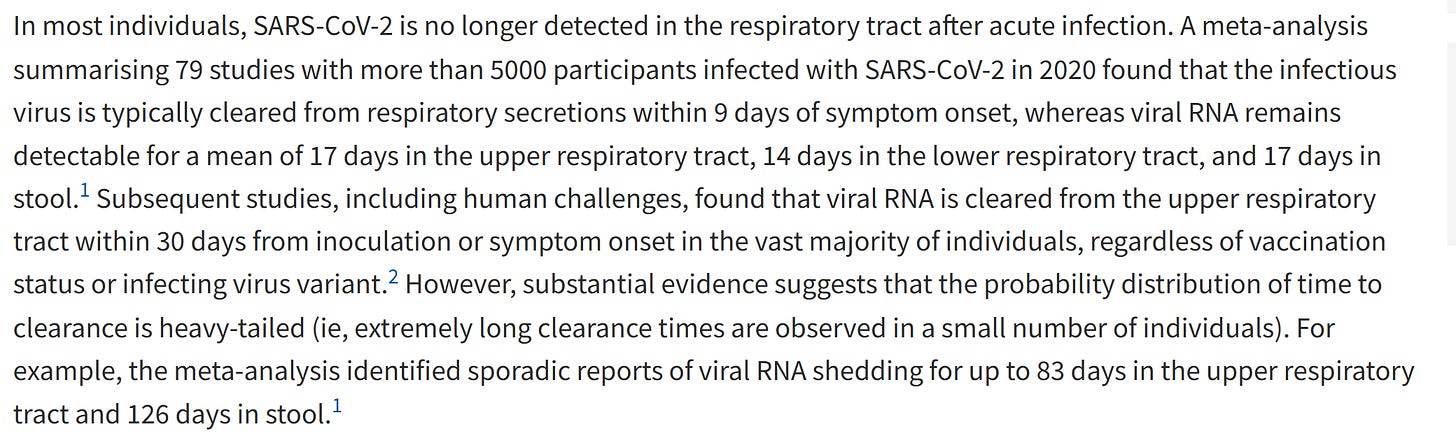
Claims of viral persistence in Long COVID: The WHN collective cites several studies to suggest that 25–60 % of Long COVID patients exhibit viral persistence. However, a closer look at the references shows:
(124): Only viral RNA detected, not infectious virus.
(125 –126): Circulating viral antigens measured, not live virus, in acute or post-acute cases.
(127): A review; no primary data, only interpreted by title.
(128): Faecal RNA shedding observed; virus infectivity was not assessed. While RNA can persist in stool, this does not equate to chronic infection, and its link to long-term gastrointestinal symptoms is unclear.
(129) Only viral antigens (protein fragments) were detected, not infectious virus. No evidence of chronic, replicating SARS-CoV-2.
(130) Post-mortem biopsies (mostly older patients with severe pneumonia) 11–300 days after infection. SARS-CoV-2 antigens were not detected in the respiratory epithelium, although some inflammatory foci contained viral debris (antigens and RNA). No infectious virus was reported, and findings correlate with disease severity and time since infection.
Conclusion: These studies do not substantiate claims of chronic infection or viral persistence in typical Long COVID patients. WHN’s reliance on RNA or antigen detection as “persistence” is misleading and scientifically unsound.
“While systemic viremia, common in untreated HIV infection, has been detected in 5–25% of Long COVID patients (121),“ this is not supported by the evidence (see above).
“By contrast, a recent small cohort study failed to detect viremia using digital transcriptomic analysis in patients with long COVID with ME/CFS at 12 months after SARS-CoV-2 infection (131).“ Yeah!! 🍾🥳 Correct use of a reference!!
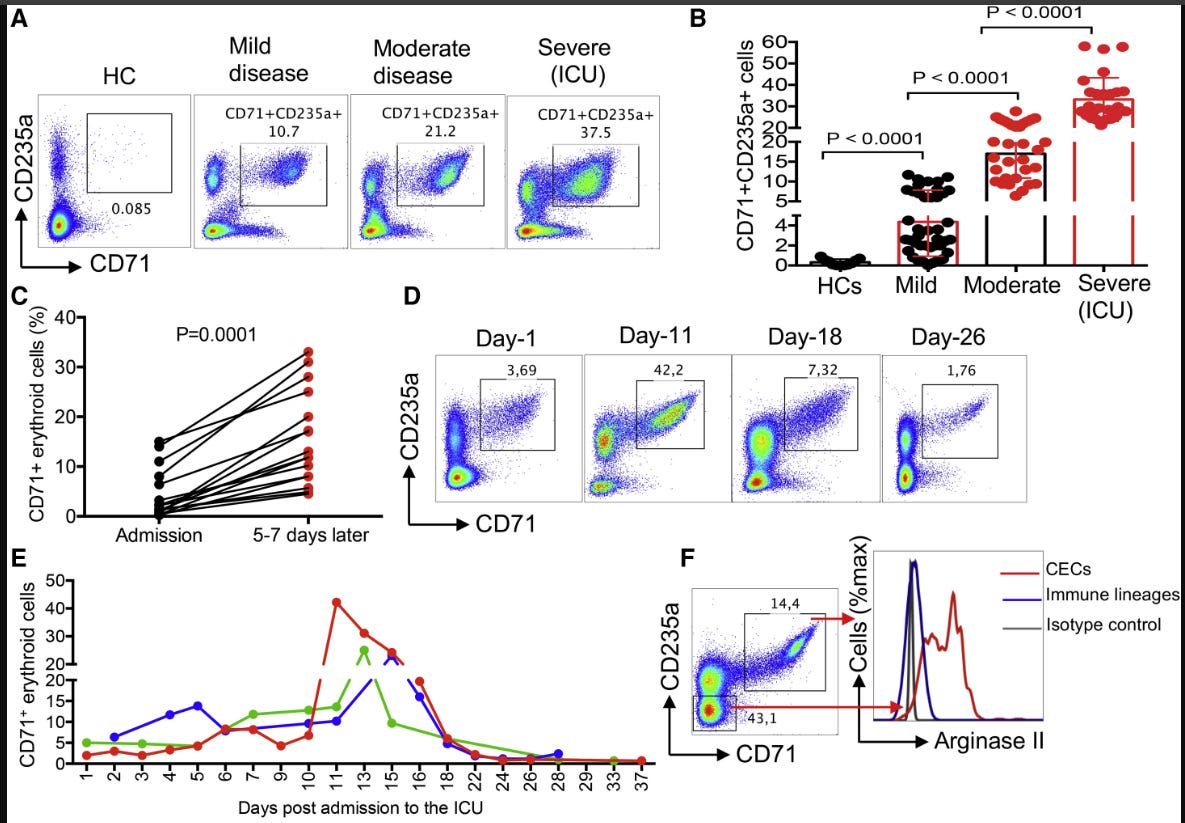
“HIV infection—and, in some reports, SARS-CoV-2 infection—has been associated with the transient expansion of erythroid progenitors/precursors, defined as CD71⁺ erythroid cells (CECs), in the periphery. These cells can modulate T cell activity and have been suggested as potential viral targets (132–134). However, the comparison between HIV and SARS-CoV-2 here is misleading. For HIV, CD4 T cells are directly depleted and reservoirs are well-established. In contrast, CEC expansion during SARS-CoV-2 infection is a physiological response to inflammation, not evidence of a persistent viral reservoir. These cells may transiently interact with the virus, but they do not serve as long-term reservoirs, and the changes resolve once the infection and inflammatory response subside.”
(133) Erythroid, red blood cell, precursors can, like any cell get infected. They are important for coagulation but also immune regulation, the observation here is something that can happen during any infection, depending on severity, and will resolve again as is shown.
(134) also supports this: there is no evidence of clinically meaningful suppression of immune function by CD71⁺ erythroid cells during SARS-CoV-2 infection. Regulatory mechanisms—including expansion of certain cell populations—occur in many infections to limit collateral tissue damage. This is a normal, protective process, not a sign of immunodeficiency. Yet the WHN collective portrays every regulatory or homeostatic mechanism as inherently dangerous, which is a profound misunderstanding of immunology.”
It is also not that they don´t know. This is done on purpose:
Another strong claim that does not align with what is actually reported in the literature cited. The WHN cherry-picks and abuses scientific literature to build up a fantasy that harms others.
Systemic Impacts and Organ Damage
HIV-1 (AIDS) – Correct. HIV infection almost inevitably leads to AIDS if untreated.
SARS-CoV-2 (PASC / Long COVID) – Can cause long-term symptoms, but this is rare. The incidence was higher during the early pandemic, when there was no pre-existing immune memory, and the immune system had to mount a strong primary response. The WHN collective misleads readers by implying that SARS-CoV-2 commonly causes a generalized, persistent immunodeficiency akin to AIDS.
The WHN claim: “Originally named after the acute respiratory syndrome caused by blood vessel damage in the lungs, SARS-CoV-2 is a primarily vascular virus” – False. The name “SARS-CoV-2,” assigned on 11 February 2020, reflects its genetic similarity to SARS-CoV, the coronavirus responsible for the 2003 SARS outbreak, not any vascular pathology.
The section immediately sets a misleading tone with a long, dramatic sentence:
“While the initial infection is often characterized by a mild, flu-like disease, especially in the post-vaccine era, it is followed by a complex chronic symptomatic condition often called Long COVID in a significant subset of patients (117, 137-139), which grows cumulatively with subsequent reinfections (23, 50, 51) and more widely in organ damage and other infection sequelae known as Post-acute Sequelae of COVID-19 (PASC) (53, 87, 140-143).”
Reality: Every viral infection can produce “flu-like” symptoms because these are driven by the immune response, not the virus itself. The claim that this is followed by a complex chronic symptomatic condition is false. Long-term symptoms occur rarely and are strongly influenced by risk factors such as severity of initial infection, female sex, and underlying health or immune conditions. If long-term symptoms are properly defined, adjusting for their baseline presence in the non-infected population, the incidence is low. Conclusion: Presenting long-term symptoms as a common or inevitable outcome of SARS-CoV-2 infection is misleading and scientifically unsupported.
The claim of a “significant subset” of patients developing Long COVID is unsupported by the references cited:
(117): A review or commentary cannot substitute for primary evidence. Using such low-level sources weakens the claim.
(137): This study examines breakthrough infections in a cohort with high baseline illness and symptom burden. It does not compare primary vs. secondary infections and provides no meaningful data on Long COVID incidence.
(138): Only 127 cases were included, with follow-up just 29 days post-infection, during a period without immune memory (Aug 2020–Mar 2021). Reporting 50% incidence is a major 🚩, not reliable evidence.
(139): Essentially a highlight of reference (137), again unrelated to the claim. Using it twice shows Google-based citation rather than proper scientific assessment.
The WHN authors make another leap of faith, asserting that long-term symptoms are “often due to persistent infection of tissue reservoirs” (120, 122, 123, 130, 144), claiming that the virus remains detectable even months after infection.
Problem: The references they cite do not support this claim. They simply repeat previously misused papers.
(144): Ironically, this paper is actually sound and clearly states that most people clear the virus, with minor variations in clearance speed. This is expected and does not support persistent infection as a cause of long-term symptoms.
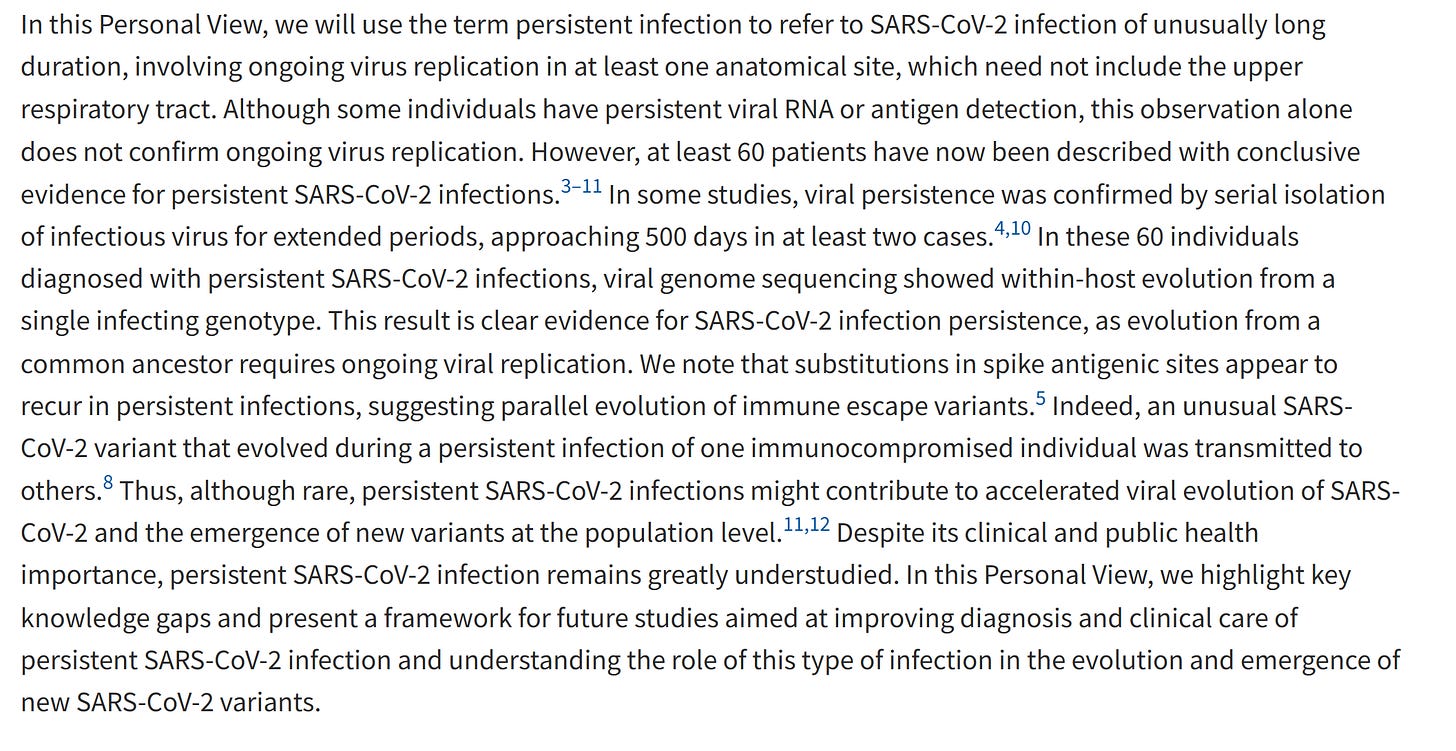
Yes, there are reports of persistent SARS-CoV-2 infection in about 60 patients. But does this substantiate the WHN claims? Absolutely not. These individuals are severely immunocompromised, unable to clear the virus, completely unlike the general population or typical Long COVID patients. They do not exhibit classic long-COVID symptoms; what is observed is intra-host viral evolution, which is a known phenomenon for many pathogens. Importantly, such cases contributed to the emergence of variants like Alpha and Omicron, but they cannot be extrapolated to claim that SARS-CoV-2 generally persists or causes chronic immune dysfunction.
Persistent SARS-CoV-2 infection is possible, particularly in severely immunocompromised individuals, and can drive rapid viral evolution. However, this undermines the WHN claims, because these chronically infected patients do not develop classic Long COVID symptoms. A likely explanation is that they lack the inflammatory responses that are thought to contribute to long-term symptoms, highlighting that it is immune-mediated effects, not the virus itself, that underlie Long COVID. The WHN’s citation of this paper appears to be driven by a Google search hit, rather than a careful reading of the actual data.
The WHN authors devote a paragraph to highlighting differences between HIV and SARS-CoV-2, which ironically confirms that their title and framing are primarily clickbait. Yet, throughout the paper and in online communications, they maintain this misleading frame, repeatedly emphasizing microclots, clearly to promote one of the co-author’s work. While microclots may plausibly contribute to symptoms, a far more credible hypothesis than “immunocompromised” or “immune damage”, they quickly move past this and return to their broader narrative.
They then attempt a link with ME/CFS, grudgingly acknowledging that similar symptoms occur following many other pathogens. This implies that Long COVID is unlikely to result from a pathogen-specific effect or irreversible immune damage, unless they intend to claim that all other viruses, bacteria, and parasites similarly cause “AIDS”, a clearly untenable position.
The section concludes with a table trying to equate AIDS and Long COVID, now limited to Long COVID, claiming “quality of life comparable to stage 4 cancer.” While this may apply to a minority of patients, it is not representative of the majority, especially among those included in high-incidence studies reporting only mild symptoms, such as a cough or sleep difficulties. Once again, the WHN authors are cherry-picking extreme cases to make their narrative appear more dramatic.
Neurological Impacts and Cognitive Decline: Comparing HAND in HIV/AIDS and SAND in SARS-CoV-2/Long COVID/PASC
The WHN authors introduce SARS-CoV-2-associated neurocognitive disorders (SAND), describing cognitive impairments such as memory loss, concentration problems, and difficulties with decision-making. While these observations are accurate, they are not unique to SARS-CoV-2. Many infections—Influenza, Influenza, Cold viruses general explanation, Sepsis, after ICU, HSV and arboviruses, HSV, general viral infections, etc—or systemic insults such as sepsis or ICU stays, and even trauma, can transiently affect brain function via inflammatory pathways. The section on “Inflammation” in the cited review provides a useful framework for understanding these risk factors.
Thus, while infections, including SARS-CoV-2, can have mild and generally temporary effects on cognition, extrapolating this to suggest a fundamental similarity with HIV/AIDS is scientifically incorrect. The authors’ attempt to amplify the scare factor by referencing Alzheimer’s Disease (AD) is misleading. Although infections may contribute to AD risk, most notably in older populations (around age 60), as observed for VZV and Influenza, vaccination programmes have mitigated this effect. Linking SARS-CoV-2 to AD in otherwise healthy, younger populations is unsupported speculation.
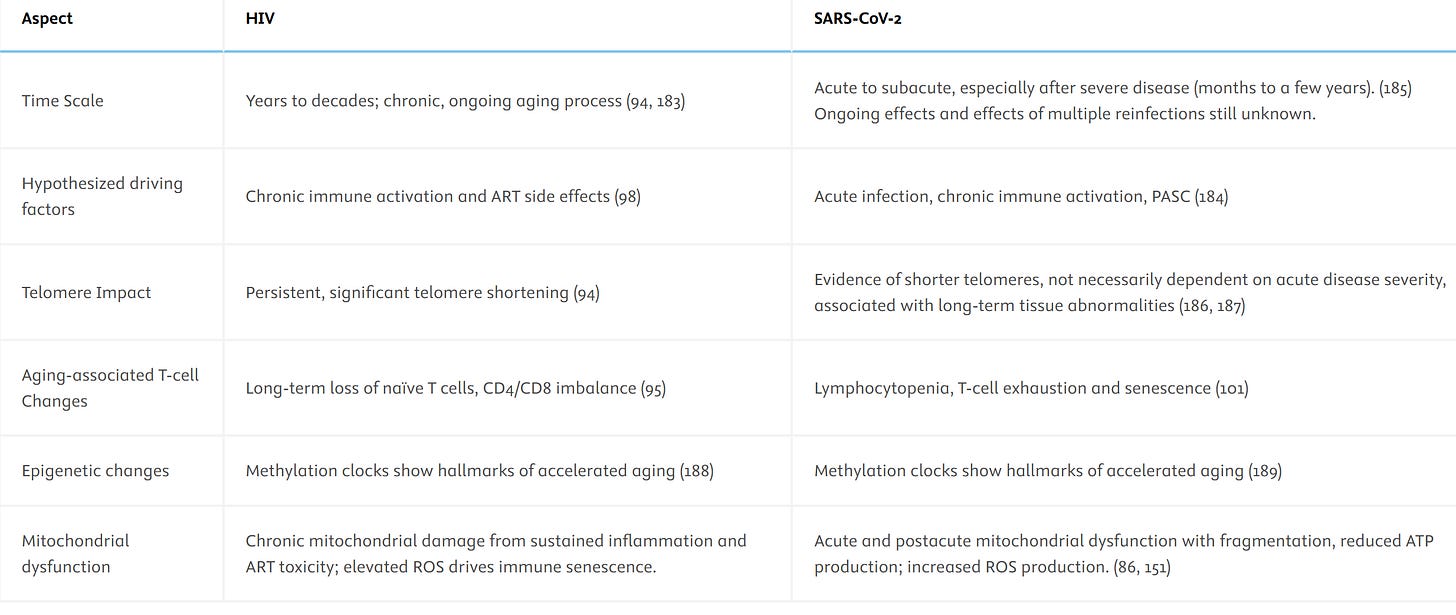
Accelerated senescence and immune exhaustion in HIV and SARS-CoV-2
The WHN section attempts to draw parallels between HIV-induced immune exhaustion and purported SARS-CoV-2-induced immune senescence. The framing is misleading and largely unsupported by the cited literature.
“SARS-CoV-2 can rapidly trigger signs of early senescence in CD4 and CD8 cells, as well as epigenetic, mitochondrial and other aging markers, even after initially mild infections (101)“ (101) Hospitalized severe COVID-19 patients, mostly elderly. Observed senescent cells and functional changes reflect age and disease severity, not virus-induced acceleration of immune aging. Temporary phenomenon, fully reversible in survivors.
Then the are more strong, but very wrong, claims and a table. So strap in, we look at all of them.
”Both viruses ultimately lead to premature exhaustion of immune resources, increasing vulnerability to age-related diseases (94, 95, 182, 183). The slow, progressive damage of HIV contrasts with the rapid onset premature aging signs in SARS-CoV-2 survivors, particularly concerning for those with multiple reinfections (87, 184).”
(94) HIV paper, I will leave those out.
(95) HIV elderly.
(182) A review/opinion. It deals with general principles, no evidence concerning anything specific for SARS-CoV-2.
(183) HIV again.
(87) As previously; A paper about SARS-CoV-2 and the DDR mechanism in Huh7 cells. Nothing to do with immunocompromised status or ageing or reinfections. Level of evidence: 0
(184) If you had not guessed it yet: another review/opinion. The WHN collective have Googled their references again, there is nothing but some suggestive titles.
The level of evidence has remained 0. Lets have a look at that table. Table 3: Accelerated senescence mechanisms in HIV and SARS-CoV-2 infections.
Again, I will limit myself to SARS-CoV-2.
(185) The authors examined blood cells from patients with severe COVID-19, observing high proliferation of immune cells. While this may appear as accelerated ageing, it primarily reflects the short-lived effector cells responding to acute infection. Memory cells that persist after the infection do not show signs of ageing. Therefore, there is no evidence of long-term immune senescence in recovered individuals.
This is an example of misinterpreting a normal, transient immune response as chronic immune ageing.
(184) An opinion/review again.
(186) As with (185) lymphocytes, SARS-CoV-2-specific, proliferate fast. Most, SARS-CoV-2-specific, die as is physiological. Their telomer length has no negative consequence to general ageing or their generation of memory T cells. Those that become memory lengthen them again. These are rescued (general highlight). Isn´t it strange how the WHN collective doesn´t include any of these excellent papers? Although a little less important for this, this can also be seen in mice (general highlight).
(187) MDPI, Same issues as the papers above, blood was used, no indication from which time during or after the infection. In addition, DNA methylation does not mean age. There is a correlation, but what it means is far from clear. Evidence for accelerated ageing: 0
(101) As above, no evidence for the claims made in this paper.
(189) A review/opinion. The WHN really don´t seem to be able to substantiate their claims with any data.
(86) Review (see earlier)! It discusses the potential involvement, of mitochondria during the infection and possibly in long-term symptoms.
(152) Predator journal …. and…. review/opinion.
Sociopolitical and economic contexts of two pandemics
“Social media has indeed amplified both information and conspiracy theories”, and the WHN has been one of the main drivers of the latter.
Their claim of ‘ongoing and significant harms caused by the pandemic’ is misleading. The pandemic ended in 2022, and the global health emergency was officially declared over in May 2023. SARS-CoV-2 is now endemic, alongside RSV, influenza, adenoviruses, and other common respiratory pathogens. Some individuals will, as always, be affected more severely, but that does not mean a pandemic is ongoing. By the same logic, we would still be in the 1918 H1N1 ‘Spanish flu’ pandemic.
Most of the global population now has robust immunity, and vulnerable groups are protected through annual boosters, just as with influenza. We have effectively replaced one virus (influenza B/Yamagata) with another (a fifth endemic coronavirus). These are facts, not minimisation.
It is understandable that people suffering from long-term symptoms seek answers, the lack of effective treatments is deeply frustrating. But spreading misinformation, misinterpreting literature, and rejecting established science only harms those patients further. The ‘airborne AIDS’ narrative is not advocacy; it is anti-science.
For some time, COVID-19 doom groups have employed the same tactics as anti-vaccine movements. Both fringe communities erode public trust, damage institutions, and undermine science itself. Increasingly, some even deny that HIV causes AIDS, a descent into pure pseudoscience.
The irony is tragic: those claiming to speak for Long COVID patients are, through disinformation and personal attacks on scientists, causing the greatest harm to the very people they claim to defend.”
Discussion
The WHN authors begin by attempting to blur definitions between “acquired immune deficiency” (AID) and HIV/AIDS, before drawing an unfounded parallel to SARS-CoV-2. This is misleading. AID is a broad category encompassing genetic disorders, immunosuppressive therapies, and chronic infections such as HIV, which causes life-long immune compromise in the absence of treatment. SARS-CoV-2, in contrast, does not induce generalized immunodeficiency. Post-infection immune function in the vast majority of recovered individuals is robust, with intact B and T cell numbers, effective memory responses, and preserved immunity to other pathogens. Attempts to label SARS-CoV-2 as “airborne AIDS” or “airborne HIV” exaggerate and misrepresent the underlying biology.
The claim that SARS-CoV-2 establishes persistent tissue reservoirs like HIV is unsupported. References cited (127, 120, 122, 123, 130) primarily detect viral RNA or protein fragments, not viable virus. Persistent infection has been observed almost exclusively in severely immunocompromised patients, not in the general population. Autopsy studies of fatal COVID-19 cases cannot be extrapolated to the majority of infected individuals, who clear the virus efficiently. Unlike HIV, which integrates into host DNA and establishes life-long reservoirs, SARS-CoV-2 is cleared in most people, negating any analogy with chronic immune suppression.
WHN repeatedly cites T cell depletion, exhaustion, and “accelerated aging” as evidence of SARS-CoV-2-induced immune deficiency. Most of these references involve hospitalized patients with severe acute disease or those with Long COVID symptoms. Transient lymphopenia, altered activation markers, or proliferation of short-lived cells during acute infection reflect normal physiological responses to viral challenge and stress. Longitudinal studies consistently show recovery of immune cell numbers and function. There is no evidence for persistent, population-wide immune dysfunction.
The suggestion that SARS-CoV-2 increases susceptibility to opportunistic infections or cancer is equally flawed. Most cited studies involve small case series, immunosuppressed patients, or reviews lacking primary data. Infections like mucormycosis, candidiasis, or tuberculosis occurred almost exclusively in patients treated with corticosteroids, with comorbidities, or severely ill, none of which indicate virus-induced generalized immunodeficiency. Similarly, no credible evidence links SARS-CoV-2 to increased cancer incidence in otherwise healthy individuals.
Neurocognitive effects and Long COVID are rare, multifactorial, and largely associated with severe disease or high inflammatory burden. While transient cognitive impairments may occur, similar patterns are observed after other viral infections (influenza, HSV, arboviruses), sepsis, or critical illness. Extrapolating these effects to suggest HIV-like neurocognitive decline is scientifically untenable. The risk is largely overblown in WHN’s narrative.
WHN’s statements on waning antibodies and “rapidly diminishing hybrid immunity” misrepresent immunology. Decline of neutralizing antibodies is expected and physiological; memory B and T cells remain effective and rapidly respond upon re-exposure, reducing disease severity. This is a universal feature of adaptive immunity and does not equate to immune suppression.
Claims of population-level vulnerability to infectious diseases due to SARS-CoV-2 are not supported by epidemiological data. By 2022, widespread immunity from infection and vaccination, together with stabilizing incidence of severe disease, shows that the virus is behaving similarly to other endemic respiratory pathogens. There is no evidence of SARS-CoV-2-induced generalized immune deficiency affecting public health at the population level.
Finally, WHN’s emphasis on systemic effects, endothelialitis, thrombosis, dysbiosis, and immune dysregulation, misrepresents normal post-infection immune responses. These inflammatory phenomena are transient, self-limited, and rarely result in lasting immune impairment. The references do not substantiate claims of chronic, virus-specific immune damage akin to HIV/AIDS.
In summary, SARS-CoV-2 does not cause acquired immunodeficiency, opportunistic infections, or AIDS-like syndromes. Comparisons to HIV/AIDS are misleading, based on selective interpretation or misreading of references, and exaggerate the risks of SARS-CoV-2 infection. Post-infection immune competence is preserved in most individuals, and transient immune changes during acute disease are physiological, not pathological. Alarmist terminology such as “airborne AIDS” misinforms the public and undermines trust in both science and public health.
Conclusions
The WHN conclusions are fundamentally flawed and misrepresent immunology, virology, and public health.
First, the statement that SARS-CoV-2 induces immune dysfunction comparable to HIV/AIDS is incorrect. T cell depletion during acute COVID-19 occurs mainly in severely ill hospitalized patients and is transient. Longitudinal studies demonstrate that T and B cell numbers, function, and memory responses recover fully in most individuals. There is no evidence that SARS-CoV-2 causes generalized immunodeficiency or opportunistic infections in the population. Cases cited are either confounded by comorbidities, immunosuppressive treatments, or extreme severity, none of which reflect typical COVID-19 infections.
Claims of “accelerated biological aging” and neurological or systemic damage are overstated. Observed alterations in immune markers, cell proliferation, or cognitive function reflect physiological stress responses or temporary inflammatory effects. Similar patterns are seen after influenza, sepsis, or other viral infections. There is no evidence of persistent virus-induced immune compromise or population-level vulnerability akin to HIV/AIDS.
The idea of “subacute and chronic persistence” of SARS-CoV-2 in tissues is unsupported in the general population. Most references cited detect viral RNA or protein fragments, not viable virus, and persistent infection is almost exclusively observed in severely immunocompromised patients. Extrapolating autopsy or immunodeficient cohort data to healthy individuals is scientifically unjustified.
The conclusions also exaggerate the public health threat. By 2022, widespread immunity from infection and vaccination significantly reduces severe outcomes, hospitalization, and transmission. SARS-CoV-2 behaves as an endemic respiratory virus in most populations. Population-level immune dysfunction does not occur. Standard hygienic, evidence-based infection control, vaccination, and patient care are sufficient to manage risks, without resorting to alarmist analogies to HIV/AIDS.
Finally, applying lessons from HIV/AIDS is only relevant insofar as general pandemic preparedness, epidemiological surveillance, and equitable patient care are concerned, not because SARS-CoV-2 causes comparable immune deficits. The WHN’s framing of SARS-CoV-2 as a virus causing long-term, population-wide immunodeficiency misleads clinicians, policymakers, and the public, and risks eroding trust in science and public health guidance.
In summary: SARS-CoV-2 does not induce HIV-like immune deficiency. Acute changes during severe infection are largely transient, long-term immune competence is preserved, and population-level vulnerability to opportunistic infections is not observed. Alarmist terminology and false equivalences with HIV/AIDS are unsupported, misleading, and scientifically indefensible.
The aims are clear: scare everyone, spread their anti-science narrative.